South Dakota is the 39th state to expand Medicaid eligibility to cover low-income adults, with coverage that could take effect as early as July 1. Applications were accepted starting June 1, and enrollment continues year-round.
What are the new Medicaid eligibility guidelines after expansion?
South Dakota's Medicaid expansion makes coverage available to many low-income adults who weren’t previously eligible and now meet eligibility criteria. This includes adults who:
- Are under age 65.
- Have a household income up to 138% of the poverty level. (For a single person, that’s $20,120 in 2023; for a household of four, it’s $41,400.)
- Are not eligible for or enrolled in Medicare.
- Are lawfully present in South Dakota and have or have applied for a Social Security number.
- Have been lawfully present in the U.S. for at least five years. (Low-income lawfully present immigrants who have been in the U.S. for any amount of time are eligible for premium subsidies in the Marketplace instead.)
Previously, non-disabled adults under age 65 were only eligible for South Dakota Medicaid if they had minor children and a household income that didn’t exceed 46% of the poverty level. (For a household of two, that was just over $9,000 in total annual income.)
Who became newly eligible for Medicaid in South Dakota as a result of expansion?
As a result of Medicaid expansion, an estimated 52,000 low-income adults in South Dakota are newly eligible for Medicaid as of July 2023.
This includes parents/caretakers with income above 46% and not more than 138% of the poverty level, as well as childless adults with income up to 138% of the poverty level.
Can I apply for expanded Medicaid if I recently lost Medicaid in South Dakota?
Yes, some people who have recently lost Medicaid in South Dakota will find that they’re once again eligible for coverage under the new guidelines.
During the COVID pandemic, states could not disenroll anyone from Medicaid unless they moved out of state, passed away, or requested a disenrollment. But that rule ended April 1, 2023 and South Dakota was among the first states to begin disenrolling people. South Dakota Medicaid enrollment dropped by more than 21,000 people by May, after just two months of disenrollments (enrollment in March was nearly 153,000, and by May it had dropped to under 132,000).
If you’ve recently been disenrolled from South Dakota Medicaid, you may have already received a notification from the state about your potential eligibility for Medicaid expansion and a reminder to submit an application.
Will Medicaid expansion affect South Dakotans who currently have Marketplace plans?
Some people who currently have subsidized private coverage through the South Dakota Marketplace will be newly eligible for expanded Medicaid as of July 1.
In addition to the non-disabled adults without minor children described above, this includes adult parents and caretakers with household income between 100% and 138% of the poverty level. For a single person, that’s between $14,580 and $20,120 in annual income this year. The amount increases if there are more people in the household.
These individuals were eligible for Marketplace subsidies to purchase private plans prior to July 1, 2023. And they will not automatically be transitioned to Medicaid in July. They’ll have the option to keep their Marketplace coverage (and subsidy) through the end of the year.
Or they can choose to apply for Medicaid and then drop their Marketplace plan if and when they’re approved for Medicaid. It’s important to wait until the Medicaid application is approved before dropping a Marketplace plan to prevent a gap in coverage. There would not be an opportunity to re-enroll in the Marketplace plan prior to January 1 unless the person has another qualifying life event.
For people in this income range who have Marketplace coverage and choose to keep it for now, Medicaid eligibility will be redetermined during open enrollment this fall. At that point, if a person is eligible for Medicaid (i.e. income up to 138% of the poverty level), they will be notified that they are no longer eligible for a subsidy in the Marketplace after the end of 2023, and are instead eligible for Medicaid.
People whose projected 2024 income is above 138% of the poverty level will continue to be eligible for subsidies in the Marketplace, as long as they can provide any requested income verification documentation. (There is no set upper income limit for subsidy eligibility. Subsidies are available as long as the benchmark plan would cost more than 8.5% of your household income.)
Which states might implement Medicaid expansion next?
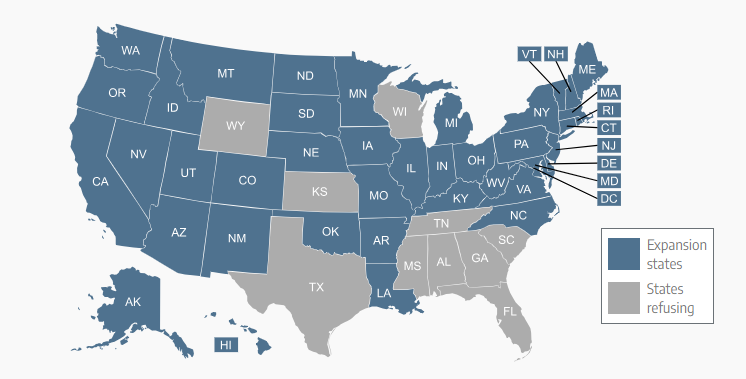
South Dakota was the 39th state to expand Medicaid, leaving 11 others that have not yet done so. North Carolina appears likely to be the next state to expand Medicaid, with coverage expected to become available in late 2023 or early 2024.
Most of the states that have expanded Medicaid in the last few years have done so as a result of voter-approved ballot measures. But those are not an option in most of the 11 remaining states, and are unlikely to be a successful strategy in the states where they are possible.
North Carolina was the first state in several years to approve Medicaid expansion legislatively, and some of the remaining states might follow suit in the coming years. Other states – including Wyoming and Kansas – have seen multiple failed attempts in the past five years to advance expansion legislation
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org since 2013. Her state health exchange updates are regularly cited by media who cover health reform and by other health insurance experts.
