Medicaid eligibility and enrollment in Delaware

Delaware’s Medicaid enrollment is 33% higher than it was in 2013, but more than 43,000 people have been disenrolled since mid-2023.

Who is eligible for Medicaid in Delaware?
The following eligibility levels apply to Delaware’s Medicaid program (for adults under age 65, pregnant women, and children, a 5% income disregard is included in these limits).
- Children birth to 1 year with family income up to 217% of the federal poverty level (FPL)
- Children 1 to 5 years with family income up to 147% of FPL
- Children 6 to 18 with family income up to 138% of FPL
- Children ages 1 to 18 who aren’t eligible for Medicaid but whose household income doesn’t exceed 217% of FPL, are covered through the Healthy Children program, which is Delaware’s Children’s Health Insurance Program
- Pregnant women with family income up to 217% of FPL (coverage for the mother continues for 12 months after the baby is born)1
- Adults under age 65 with family income up to 138% of FPL (Medicaid expansion population)
- Elderly and disabled individuals with special requirements and who meet certain income and asset limits. Use Delaware ASSIST (Application for Social Services and Internet Screening Tool) to see if you qualify.
Apply for Medicaid in Delaware
Online at HealthCare.gov or through Delaware ASSIST; by mail (call 1-800-372-2022 or 302-255-9500 to have an application mailed to you); in person (Call 1-800-372-2022 or 302-255-9500 to be directed to the nearest DSS office.) To apply for long-term care, call the Nursing Facility Program Eligibility Unit for your county.
Eligibility: Children birth to 1 year with family income up to 212% of FPL; children 1-5 years with family income up to 142% of FPL; children 6-18 with family income up to 138% of FPL; pregnant women with family income up to 212% of FPL; parents with family income up to 138% of FPL; childless, non-elderly adults with family income up to 138% of FPL; elderly and disabled individuals with special requirements and who meet certain income limits (Use Delaware ASSIST to see if you qualify.); children 1-18 up to 212% of FPL are covered through the Healthy Children.



Did Delaware expand Medicaid under the ACA?
Yes. Delaware opted to accept federal funding to expand Medicaid eligibility to adults under the age of 65 with incomes up to 138% of the federal poverty level (FPL). Coverage effective dates for those qualifying for Medicaid expansion started Jan. 1, 2014. The federal government paid the full cost of expanding coverage to the newly eligible population through 2016, although states now pay 10% of the cost.
Not coincidentally, the uninsured rate in Delaware dropped from 9.1% in 2013 to 5.7% in 2017. But it grew to 6.6% in 2019, in line with the nationwide increase in the uninsured rate under the Trump administration.
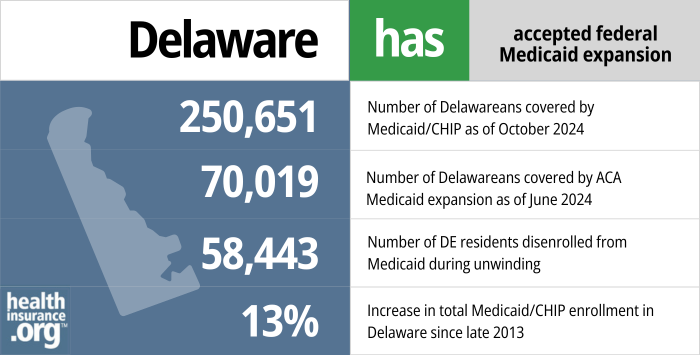
- 250,651 – Number of Delawareans covered by Medicaid/CHIP as of October 20242
- 70,019 – Number of Delawareans covered by ACA Medicaid expansion as of June 20243
- 58,443 – Number of DE residents disenrolled from Medicaid during unwinding4
- 13% – Increase in total Medicaid/CHIP enrollment in Delaware since late 20135
Explore our other comprehensive guides to coverage in Delaware

We’ve created this guide to help you understand the health insurance options available to you and your family in Delaware.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Delaware.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Delaware as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Delaware Medicaid eligibility and enrollment
How do I apply for Medicaid in Delaware?
- You can apply for Medicaid online at HealthCare.gov or through Delaware ASSIST.
- You can fill out a paper application and return it by mail. Call 1-800-372-2022 or 302-255-9500 to have an application mailed to you.
- Call 1-800-372-2022 or 302-255-9500 to be directed to the nearest DSS office.
- To apply for long-term care, call the Medicaid Central Intake Unit at 1-866-940-8963 or the Nursing Facility Program Medical Eligibility Unit for your county.
How does Medicaid provide financial assistance to Medicare beneficiaries in Delaware?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Delaware includes overviews of these programs, including Medicaid nursing home benefits, Extra Help, and eligibility guidelines for assistance.
How is Delaware handling Medicaid renewals after the pandemic?
From March 2020 through March 2023, Medicaid disenrollments were paused nationwide. Even if an enrollee’s circumstances changed and they were no longer eligible for Medicaid, their coverage remained in effect. But that continuous coverage requirement ended March 31, 2023, and states have a 12-month “unwinding” period when they must initiate eligibility redeterminations for everyone enrolled in Medicaid, and disenroll those who are no longer eligible.
States could begin the unwinding period in February, March, or April 2023, although disenrollments could not come before April 1. Delaware opted to begin the unwinding period in April 2023, with the first round of disenrollements in June.
Delaware officials expected 40,000 to 50,000 of the state’s 315,000 Medicaid/CHIP enrollees to be disenrolled during the year-long unwinding period. By January 2024, in the ninth month of disenrollments, a total of 43,449 people had been disenrolled from Delaware Medicaid.6
People will lose Medicaid/CHIP if they’re no longer eligible, but also if they fail to respond to a renewal notice from the state. As has been the case nationwide, the majority of the people disenrolled from Delaware Medicaid (more than 25,000) have been disenrolled for procedural reasons, meaning that the state didn’t have enough information to determine whether they were still eligible.6
People who lose Medicaid can transition to an employer’s plan (if available), Medicare (if eligible; with access to Medigap), or to an individual/family plan obtained through Delaware’s exchange (HealthCare.gov; assistance is available at ChooseHealthDE). By September 2023, more than 3,000 people had transitioned from Delaware Medicaid to a Marketplace plan.7
There is a 60-day window to enroll in an employer’s plan after losing Medicaid, and a six-month window to enroll in Medicare (but Delaware Medigap insurers only have to provide a 63-day guaranteed-issue window, so it’s important to enroll quickly if you’re switching to Medicare and want access to a Medigap plan). The window to enroll in an exchange/marketplace plan runs from March 31, 2023 to July 31, 2024 for people who lose Medicaid in that window. However, coverage is not retroactive, so it’s important to sign up before the date that Medicaid ends to avoid a coverage gap.
How many people are enrolled in Delaware Medicaid?
As of September 2023, total enrollment in Delaware’s Medicaid/CHIP programs was 33% higher than it had been in 2013, and stood at just under 300,000 people. Percentage-wise, this is smaller than the enrollment growth in many other states that have expanded Medicaid. But Delaware’s median household income is higher than the national average, so fewer people are eligible for coverage intended for low-income households
Nationwide, total Medicaid/CHIP enrollment is up 54% from where it stood in late 2013, with significant enrollment growth since 2020 as a result of the COVID pandemic and the pause on Medicaid disenrollments between March 2020 and March 2023. But Medicaid enrollment has been declining nationwide (and in Delaware) since early/mid-2023, due to the end of the pandemic-related continuous coverage rule.
Legislation impacting Delaware Medicaid
Delaware Medicaid history
Delaware originally implemented Medicaid in October 1966.
Starting in 1996, the state began converting much of its program to managed care, contracting with managed care organizations (MCOs) to provide Medicaid benefits. The state currently contracts with three MCOs (AmeriHealth Caritas Delaware, Highmark Health Options, and Delaware First Health) to provide Medicaid benefits to eligible enrollees.
In April 2012, Delaware received approval to move some of its long-term care and dual-eligible (those who qualify for both Medicaid and Medicare) populations to managed care. This program is called DSHP Plus. About 85% of Delaware’s Medicaid enrollees are covered under managed care plans, including DSHP Plus.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Delaware Extends Postpartum Medicaid Coverage to 12 months. Delaware Division of Medicaid and Medical Assistance. June 2023. ⤶
- October 2024 Medicaid & CHIP Enrollment Data Highlights, Medicaid.gov, Accessed January 2025 ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment, Medicaid.gov, Accessed February 2025 ⤶
- Medicaid Continuous Coverage Unwinding Renewals Reporting, dhss.delaware.gov, Accessed January 2025 ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment, KFF.org, Accessed February 2025 ⤶
- Medicaid Continuous Coverage Unwinding Renewals Reporting, dhss.delaware.gov, January 2024. ⤶ ⤶
- HealthCare.gov Marketplace Medicaid Unwinding Report. Centers for Medicare and Medicaid Services. Data through September 2023. ⤶

