In this article
Twelve of the states that have expanded Medicaid under the Affordable Care Act (ACA) have so-called “trigger laws” in place that would quickly end or potentially scale back Medicaid expansion if the share of federal funding for Medicaid expansion drops. Here’s what you need to know about these trigger laws and the states that would likely be affected:
How federal funding of Medicaid expansion works
Under the Affordable Care Act and a subsequent Supreme Court ruling, states have the option to expand Medicaid eligibility to include low-income adults (up to 138% of the federal poverty level), in addition to the populations that were traditionally eligible for Medicaid (low-income children, pregnant women, senior citizens, and disabled people). If a state implements Medicaid expansion, the federal government pays 90% of the cost of covering the expansion population, while states pay 10% of the cost.1
This is much higher than the federal funding rate that applies to the rest of the Medicaid population, which is a minimum of 50% and a maximum of 83%. In FY2025, federal funding ranged from 50% (10 states) to 77.27% (Mississippi), and as high as 83% in some of the U.S. territories.2 The formula is designed so that the federal government pays a larger portion of Medicaid costs in states with lower per capita incomes relative to the national average.3
So it’s quite a bit less expensive for states to cover a person in the Medicaid expansion population than to cover a member of their traditional Medicaid population (children and people over age 65, as well as some adults who are pregnant or disabled and not eligible under the Medicaid expansion guidelines).
For perspective, the total Medicaid population as of late 2024 – including the Medicaid expansion population – was about 72 million people (in addition to more than 7 million enrolled in CHIP).4 Medicaid expansion enrollment stood at just under 21 million people as of mid-2024.5 For those 21 million people, the federal government was funding 90% of the cost of their coverage. The rest of the Medicaid population is enrolled under traditional eligibility pathways, with the federal government funding a lower share of the cost of their coverage.
What are Medicaid trigger laws?
Several states – listed below – have laws in place that will automatically terminate Medicaid expansion in these states if the federal matching percentage is reduced.
This means enrollees with Medicaid expansion coverage would lose their coverage soon after a reduction in federal funding.6
There are variations in terms of the specific state rules. For example, the trigger law in Illinois calls for Medicaid expansion eligibility to end “no later than the end of the third month following” the month the federal funding reduction takes effect.7 And in Arkansas, the trigger law calls for the state to transition enrollees out of the Medicaid expansion program within 120 days of the federal funding reduction.8
But in Arizona, the state’s trigger law simply says that the state “shall discontinue eligibility” under Medicaid expansion if federal funding drops below 80%, without a set waiting period before that takes effect. (Arizona’s trigger law has an 80% threshold rather than 90%.)9 And in Utah, the trigger law would end Medicaid expansion “no later than the next July 1” after the date the federal funding is reduced.10 Depending on the timing of a federal funding cut, that could be an almost immediate termination of Medicaid expansion, or there could be a delay of up to almost a year.
If a trigger law is activated and Medicaid expansion ends, access to coverage in the state would then work the way it does in the states that haven’t expanded Medicaid. There would be a coverage gap for most adults with income below the federal poverty level, and Marketplace subsidy eligibility would begin at household incomes equal to the federal poverty level (FPL). While Medicaid expansion is in place, Marketplace subsidy eligibility begins with household incomes above 138% of FPL because residents in expansion states are eligible for Medicaid if they have a household income up to 138% of FPL.
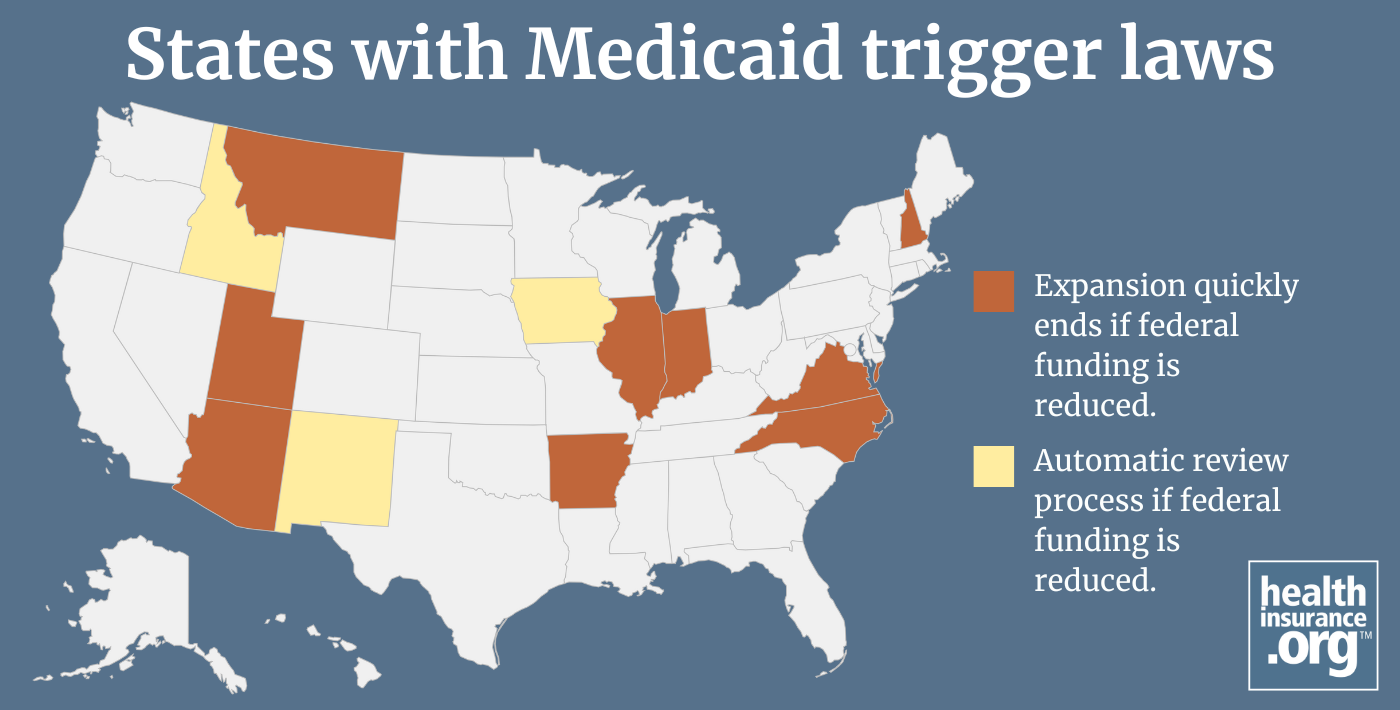
Which states have trigger laws?
The states with trigger laws are:6
- Arizona (Expansion would end if the federal match drops below 80%.)9
- Arkansas
- Illinois (Legislation introduced in 2025 would remove the trigger law.)11
- Indiana
- Montana
- New Hampshire
- North Carolina (Legislation introduced in 202512 would change the trigger law so that it would only be activated if the federal matching rate for the expansion population were to drop below the federal matching rate for the rest of the Medicaid population, which is currently about 65% in North Carolina.13)
- Utah
- Virginia (A 2025 Virginia budget amendment that would have developed “recommendations to preserve health care access to as many Medicaid members as possible”14 was not included in the state's budget, but if federal funding for Medicaid expansion is reduced, Virginia’s Legislature can reconvene for a special session.)15
Another three states – Iowa, Idaho, and New Mexico – have rules in place that would trigger a review of Medicaid expansion if the federal match rate were to drop below 90%. So while these states do have trigger laws, the trigger is for a review of the program rather than an automatic termination. But that review could result in benefit cuts or the elimination of Medicaid expansion.6
Idaho enacted legislation in 2025 to clarify that if federal Medicaid expansion funding were to be reduced when the state legislature isn't in session, the Idaho Department of Health & Welfare "shall take any action necessary to offset the increase in state funding, including but not limited to reductions in provider payment rates or elimination of optional benefits."16
How many people would lose Medicaid coverage due to trigger laws?
More than 3 million people would lose their health coverage if the federal matching rate were to be reduced and the state trigger laws were to be activated. That number would increase to almost 3.7 million if Medicaid expansion were to also be eliminated in Iowa, Idaho, and New Mexico.6
How would states without trigger laws be affected if federal Medicaid funding is reduced?
It would likely be difficult for any Medicaid expansion state to pick up the slack if federal Medicaid funding for the expansion population is reduced. If that happens, expansion states without trigger laws might enact legislation to change or eliminate their Medicaid expansion programs.
South Dakota’s legislature enacted a joint resolution in March 2025 that calls for a measure to be placed on the state ballot allowing voters to decide whether Medicaid expansion in the state should continue if federal funding drops below 90%.17
Lawmakers in West Virginia and Idaho are considering legislation in 2025 that would create trigger laws in those states. The legislation in West Virginia was introduced in late March and was under consideration by the state House in early April.18 The legislation in Idaho passed in the state House in February and was sent to the Senate for consideration.19
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written hundreds of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “Title 42 § 433.10 Rates of FFP for program services (subsection c(6)(i))” Code of Federal Regulations. Accessed Mar. 10, 2025 ⤶
- “EXHIBIT 6. Federal Medical Assistance Percentages and Enhanced Federal Medical Assistance Percentages by State, FYs 2022–2025” MACPAC.gov. Accessed Mar. 24, 2025 ⤶
- “Medicaid’s Federal Medical Assistance Percentage (FMAP)” Congressional Research Service. July 29, 2020 ⤶
- “October 2024 Medicaid & CHIP Enrollment Data Highlights” Medicaid.gov. Accessed Mar. 24, 2025 ⤶
- “Medicaid Enrollment - New Adult Group” Medicaid.gov. Accessed Mar. 24, 2025 ⤶
- “Federal Funding Cuts to Medicaid May Trigger Automatic Loss of Health Coverage for Millions of Residents of Certain States” Georgetown University Center for Children and Families. Nov. 27, 2024 ⤶ ⤶ ⤶ ⤶
- “305 ILCS 5/5-2 (18)” Illinois General Assembly. Accessed Mar. 24, 2025 ⤶
- “AR Code § 23-61-1004 (2024)” Justia Law. Accessed Mar. 25, 2025 ⤶
- “2024 Arizona Revised Statutes, Title 36 - Public Health and Safety § 36-2901.07 - Definition of eligible person; conditional eligibility” (Subsection B) Justia Law. Accessed Mar. 14, 2025 ⤶ ⤶
- “26B-3-210(5)” Utah State Legislature. Accessed Mar. 25, 2025 ⤶
- “Illinois HB3998” BillTrack50. Introduced Feb. 27, 2025 ⤶
- "North Carolina H653" BillTrack50. In committee Apr. 2, 2025 ⤶
- "EXHIBIT 6. Federal Medical Assistance Percentages and Enhanced Federal Medical Assistance Percentages by State, FYs 2022–2025" MACPAC.gov. Accessed Apr. 6, 2025 ⤶
- “Budget Amendments - SB800 (Member Request)” Virginia State Budget, 2025 Session. Accessed Mar. 3, 2025 ⤶
- “Medicaid expansion trigger law left untouched during General Assembly” VPM.org. Feb. 26, 2025 ⤶
- "Idaho H345" BillTrack50. Enacted Mar. 20, 2025 ⤶
- “South Dakota HJR5001” BillTrack50. Enacted Mar. 6, 2025 ⤶
- "West Virginia HB3518" BillTrack50. Introduced Mar. 28, 2025 ⤶
- "Idaho H138" BillTrack50. Crossed over, Feb. 19, 2025 ⤶
Your health insurance options may depend on where you live
Find out what coverage is available in your state.


