What is a health insurance claim?
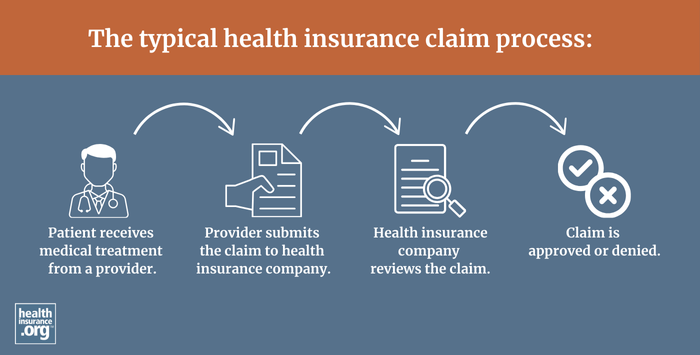
A claim is an application for benefits provided by your health plan. You or your medical provider must file a claim before funds will be reimbursed for your care. If you're using an in-network medical provider, they should file the claim on your behalf. But if you see an out-of-network provider, you may have to file the claim yourself, and you may also have to pay for the care upfront and seek reimbursement from your insurer, assuming that your plan covers out-of-network care.
Many insurers require pre-certification (prior authorization) for non-emergency treatment, which is separate from the submission of the claims. Prior authorization happens before the medical procedure is performed, whereas a claim is submitted after the care has been provided. In any case, a claim may be denied based on the carrier’s assessment of the circumstance, and there are appeals processes that patients and medical providers can use if that happens.
