What is an explanation of benefits?
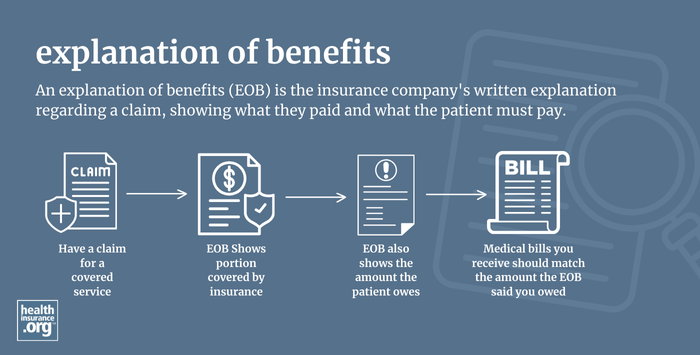
An explanation of benefits (EOB) is the insurance company's written explanation regarding a claim, showing what they paid and what the patient must pay. The document is sometimes accompanied by a benefits check, but it's much more common for the insurer to send payment directly to the medical provider (an EOB will generally only include a benefits check if the claim was out-of-network and the patient is being reimbursed by a plan that covers out-of-network care).
The EOB is not a bill, although it will explain any charges that the patient still owes or may have already paid (in the form of a copay at the time the medical care was received, for example). If the patient owes additional money after the insurance company has paid its portion, the medical provider will send a separate bill, which should match the patient's portion listed on the EOB.
As a general rule, for services that aren't covered with a copay (meaning they either count toward your deductible or you'll be paying coinsurance for the care if you've already met your deductible), you should wait to pay the medical provider until you receive an EOB from your health plan. If your share of the charges on the EOB doesn't match the bill you received from your medical provider, you should contact the provider and your health plan to make sure you understand any discrepancies and clarify how much you owe.
For services that are covered with a copay, such as office visits or prescriptions (depending on the plan), you should generally expect to have to pay your copay at the time the care is received. But you should still receive an EOB at a later date. This will let you know whether your share of the bill is just the copay that you've already paid, or if you still owe anything else.


