What does in-network mean?
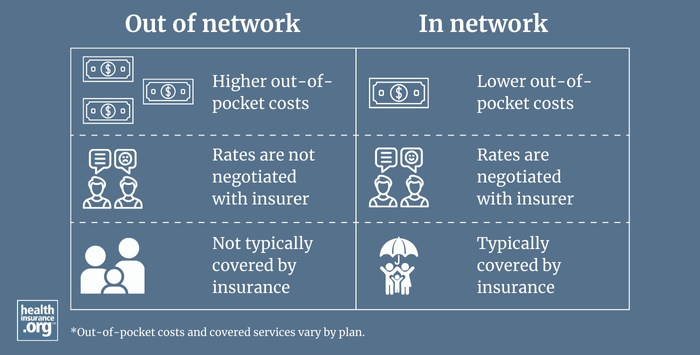
In network refers to providers or health care facilities that are part of a health plan's network of providers with which it has negotiated a discount. Insured individuals usually pay less when using an in-network provider, because those networks provide services at lower cost to the insurance companies with which they have contracts. The provider's contract with the insurer requires the insurer to accept the insurer's payment (plus the patient's cost-sharing, such as the deductible, copay, or coinsurance) as payment in full, so an in-network provider cannot balance bill a patient.
Some health plans only pay for services when the member uses in-network providers, while other health plans will pay at least some of the claim even if the member uses an out-of-network provider. But even if the health plan pays for out-of-network care, the patient's cost-sharing will be higher. And the patient will potentially be subject to balance billing, since the out-of-network provider does not have a contractual agreement with the patient's health plan.
