State-by-state Medicaid expansion guide
See if your state has expanded Medicaid eligibility, who’s eligible under expansion, and how many people have gained coverage
In this guide
- What is Medicaid expansion?
- Who’s eligible under Medicaid expansion?
- How many people are enrolled in coverage due to Medicaid expansion?
- What is the Medicaid coverage gap?
- Which states have expanded Medicaid?
- How is Medicaid expansion funded?
- Which states would automatically end Medicaid expansion if the federal funding rate is reduced?
- Legislation and ballot measures that have resulted in Medicaid expansion

What is Medicaid expansion?
Medicaid expansion was a cornerstone of the Affordable Care Act (ACA), which called for states to expand Medicaid eligibility guidelines to include adults under age 65 with household income up to 138% of the federal poverty level (regardless of assets).
Prior to 2014, low-income adults were not eligible for Medicaid in most states unless they were pregnant, disabled, or the parent/caretaker of a minor child. But the ACA’s expansion of Medicaid added a new eligibility category for low-income adults, even if they didn’t fit into one of those other categories.
As discussed below, Medicaid expansion became optional for states due to a 2012 Supreme Court ruling, and ten states have not implemented Medicaid expansion as of 2025.
Who's eligible under Medicaid expansion?
Under the expansion guidelines, Medicaid eligibility is extended to adults under age 65 with incomes up to 138% of the federal poverty level/FPL (133% plus a 5% income disregard, which means if a person’s income is no more than 5 percentage points above the eligibility threshold, they will be considered eligible for the program).1
Starting in 2027 (with some flexibility in terms of the timing of when states implement the program), there will be a nationwide work requirement for Medicaid expansion. As we get closer to 2027, Medicaid expansion enrollees will receive information from their state about the work requirement and what they’ll need to do to comply; enrollees should ensure that the state has their correct contact information on file and reach out to the state if they have any questions.
Unless they qualify for an exemption (for example, due to being medically frail or the parent/caretaker of a child age 13 or younger),2 Medicaid expansion enrollees will have to be working at least 80 hours per month (or attending school, volunteering, or participating in other allowable community engagement activities). Work hours will have to be reported to the state Medicaid agency in order to remain eligible for coverage. This requirement is due to H.R. 1, the federal legislation more commonly known as the “Big Beautiful Bill,” which was enacted in 2025.3
Before the ACA’s expansion of Medicaid became available in 2014, Medicaid was generally unavailable to non-disabled adults under age 65 unless they were pregnant or had minor children.4 And the income caps to qualify as a parent/caretaker were very low (and continue to be quite low in most of the states that haven’t expanded Medicaid).5 By providing additional funding for states to expand their Medicaid programs, the ACA created a viable pathway to public health insurance coverage for millions of low-income adults.
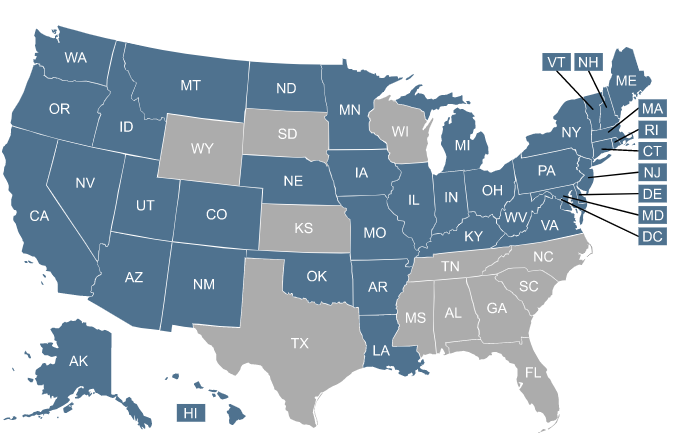
Click on the map or the list of states to learn more about Medicaid expansion in your state.
How many people are enrolled in coverage due to Medicaid expansion?
As of March 2025, Medicaid expansion enrollment stood at about 20.7 million people.6
It had been higher, at about 24.8 million people in May 2023.7 But after a three-year pandemic-related pause, Medicaid eligibility redeterminations and disenrollment resumed in 2023, in a process referred to as “unwinding.” This resulted in a significant drop in total Medicaid enrollment nationwide, including a reduction of about 4 million Medicaid expansion enrollees.
Total enrollment in Medicaid/CHIP was 35% higher in August 2025 than it had been in late 2013 (a growth of almost 21 million people),8 despite the fact that there are still ten states that haven’t expanded Medicaid, and despite the fact that the post-pandemic “unwinding” process had been completed.
What is the Medicaid coverage gap?
In nine of the ten states that have not expanded Medicaid (all but Wisconsin), there’s a coverage gap that leaves almost 1.4 million people ineligible for any sort of affordable coverage.9 These people are not eligible for premium subsidies in the Marketplace because their income is under the poverty level. But they are also ineligible for Medicaid because their states have not implemented Medicaid expansion.
According to 2023 US Census data, the uninsured rate for adults under age 65 was 8.9% in states that had expanded Medicaid, and 15.5% in states that had not expanded Medicaid.10 To be clear, this is due to the decisions that their states have made. The states could opt to implement Medicaid expansion at any time, thus closing the coverage gap. But Medicaid expansion legislation has been introduced many times over the years in the remaining non-expansion states, and has thus far been unsuccessful.
Three states – Texas, Florida, and Georgia – account for the lion’s share of the coverage gap population.9
State participation in Medicaid expansion
Which states have expanded Medicaid?
As of 2025, Medicaid has been expanded in 40 states and Washington, D.C.
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Dakota
- Utah
- Vermont
- Virginia
- Washington
- Washington, D.C. (eligibility extends to 215% FPL)11
- West Virginia
Which states have decided to not expand Medicaid eligibility?
As of 2025, the following states had not accepted federal funding to expand Medicaid:
- Alabama
- Florida
- Georgia (partial expansion took effect in mid-2023, with a work requirement)12
- Kansas
- Mississippi
- South Carolina
- Tennessee (no coverage gap for parents of minor children)13
- Texas
- Wisconsin (no coverage gap)9
- Wyoming
Why are there some states that haven't implemented Medicaid expansion?
The ACA called for Medicaid expansion nationwide. But in June 2012, the Supreme Court ruled that states could not be forced to expand their Medicaid programs,14 so it was left to each state to determine whether to participate or not.
When Medicaid expansion took effect in 2014, it was only implemented in 26 states and DC.15 In the ensuing years, there was a slow but steady increase in the number of states implementing Medicaid expansion. As of 2025, Medicaid had been expanded in 40 states and the District of Columbia (see list above). Oklahoma, Missouri, South Dakota, and North Carolina are the most recent states to have expanded Medicaid, all doing so between 2021 and 2023. But no additional states implemented Medicaid expansion in 2024 or 2025.
Wisconsin is not counted among the Medicaid expansion states, but the rules are different there. Wisconsin has implemented what essentially amounts to a partial expansion of Medicaid, and has no coverage gap because Medicaid is available to low-income adults with income below the poverty level.9
But because Wisconsin has not fully expanded Medicaid as called for in the ACA (meaning, Medicaid is not available in Wisconsin to adults with income between 100% and 138% of FPL), the state does not receive the enhanced federal Medicaid funding that it would receive if it fully expanded Medicaid.16
Georgia partially expanded Medicaid in the summer of 2023, using an approach similar to Wisconsin’s (meaning it still counts as a non-expansion state), and also incorporating a work requirement.)12 Like Wisconsin, Georgia is not receiving the enhanced federal funding that would be available if the state were to fully expand Medicaid.17 And enrollment in Georgia’s partial Medicaid expansion has been quite low, with only about 11,600 people enrolled as of November 202518 (versus more than 450,000 who would be eligible if the state adopted full Medicaid expansion without a work requirement).19
How is Medicaid expansion funded?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs for enrollees who are newly eligible under the expanded guidelines were covered 100% by the federal government until the end of 2016. The states then gradually started paying a portion of the cost, reaching 10% by 2020.20
Absent changes to the ACA, the funding will remain at the 90/10 split going forward, with the federal government always paying 90% of the cost of covering the population that became newly eligible due to the expansion of Medicaid. (As described below, some states have rules in place that would automatically end Medicaid expansion if the federal match rate were to be reduced.)
The states that refuse to expand Medicaid only receive their normal federal Medicaid funding,21 rather than the enhanced 90% funding that they would receive to cover the newly eligible population if they were to expand coverage (in the Medicaid expansion states, the normal federal funding still applies for the populations that were already eligible pre-expansion, including children, pregnant women, and low-income parent/caretaker relatives, as well as elderly, blind, and disabled enrollees whose eligibility is subject to both income and asset limits).
As noted above, the federal government does not provide the enhanced funding unless a state fully expands Medicaid. So Wisconsin and Georgia continue to receive their normal federal match for Medicaid funding, and Utah was unable to secure Medicaid expansion funding until Medicaid was fully expanded (Utah initially implemented a partial expansion of Medicaid, but did not receive enhanced federal funding for it).22
Which states would automatically end Medicaid expansion if the federal funding rate is reduced?
Under the ACA, the federal government pays 90% of the cost of covering the Medicaid expansion population, while states pay 10% of the cost. But several states have laws in place that would automatically terminate Medicaid expansion in the state if that federal matching percentage were to ever drop below 90%.23
Learn more about the 12 states whose Medicaid trigger laws would quickly end or scale back Medicaid expansion if the share of federal funding for Medicaid expansion drops. State lawmakers routinely consider legislation that could affect eligibility for and access to Medicaid benefits. Some bills would put increased limits on Medicaid eligibility while others would expand access to coverage or give currently ineligible residents a chance to buy into the Medicaid program.
Medicaid expansion legislation
Lawmakers in the states that haven’t expanded Medicaid have continued to introduce legislation each year in an effort to expand coverage. Here’s are the latest updates on that legislation:
Legislation to expand Medicaid
In 2018, Virginia lawmakers passed a budget bill that includes Medicaid expansion, with coverage that took effect in January 2019. As of July 2025, more than 613,000 people were enrolled in Virginia Medicaid under the expanded eligibility guidelines.24
Georgia enacted legislation (SB106) in 2019 that allowed the state to submit a Medicaid expansion proposal to CMS, but only for people earning up to 100% of the poverty level (as opposed to 138%, as called for in the ACA). CMS approved the partial expansion to take effect in mid-2021 but rejected the state’s request for full Medicaid expansion funding. After the Biden administration revoked approval for Georgia’s planned work requirement, the state paused implementation of the partial Medicaid expansion. It did eventually take effect in July 2023, but enrollment has remained quite low, due to the work requirement and reporting requirements that go along with it.25
From 2019 through 2022, no additional states enacted legislation to expand Medicaid. But that dry spell ended in 2023 when North Carolina enacted H.76, which called for Medicaid expansion in the state, contingent on the passage of the state’s budget bill. The budget was eventually settled in the fall, and Medicaid was expanded in North Carolina in December 2023. By December 2025, nearly 693,000 people were enrolled in expanded Medicaid in North Carolina.26
No additional states enacted Medicaid expansion in 2024 or 2025. And while the American Rescue Plan (ARP) provided a two-year additional enhancement to federal Medicaid funding for states that newly adopted Medicaid expansion, that provision was eliminated by the “One Big Beautiful Bill,” starting in 2026.27 So if any states choose to expand Medicaid in 2026 or a future year, they will get the regular 90% federal funding for the Medicaid expansion population, but not the additional federal funding that was temporarily available under the ARP.
Medicaid expansion with a ballot initiative
In Maine, Utah, Idaho, Nebraska, Oklahoma, Missouri, and South Dakota, Medicaid expansion came about as a result of ballot measures passed by voters.28
Medicaid expansion ballot initiatives have passed in 100% of the states that have had them on the ballot29 (Montana voters did not approve a 2018 measure that would have provided ongoing funding for the state’s Medicaid expansion – which was already in effect – but this did not affect the state’s Medicaid expansion, which continues to be available to eligible residents).30
But in most of the remaining non-expansion states, ballot measures to expand Medicaid are not an option.29 Medicaid expansion advocates in Mississippi had been working to gather signatures for a 2022 ballot measure,31 but suspended their campaign after a Mississippi Supreme Court decision that currently makes it impossible for a signature-gathering campaign to be successful in the state.32
There’s plenty of activity to monitor at the state level. You can click on a state on this list to see current Medicaid-related legislation:
Footnotes
- “Medicaid expansion to the new adult group” Medicaid and CHIP Payment and Access Commission (MACPAC). Mar. 30, 2023. And “With respect to MAGI conversion, how will the 5% disregard be applied?” Medicaid.gov. Accessed Aug. 18, 2025 ⤶
- “A Summary of Federal Medicaid Work Requirements” Center for Health Care Strategies. July 2025 ⤶
- “H.R.1 – One Big Beautiful Bill Act” (Section 71119). Congress.gov. Enacted July 4, 2025 ⤶
- “ACA Coverage Expansions and Low-Income Workers” KFF.org. June 10, 2016 ⤶
- “Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels” Centers for Medicare & Medicaid Services. December 2023. ⤶
- “Medicaid Enrollment – New Adult Group” (filtered for 2025, month 3). Medicaid.gov. Accessed Dec. 22, 2025 ⤶
- “Medicaid Enrollment – New Adult Group”(filtered for 2023, month 5). Medicaid.gov. Accessed Dec. 22 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” KFF.org. Accessed Dec. 22, 2025 ⤶
- “How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion?” KFF.org. Feb. 25, 2025 ⤶ ⤶ ⤶ ⤶
- ”Health Insurance Coverage in the United States: 2023” (Page 9). U.S. Census Bureau. Accessed Dec. 22, 2025 ⤶
- “Adults without Dependent Children (Childless Adults)” DC Department of Health Care Finance. Accessed Aug. 7, 2025 ⤶
- “Georgia’s Pathways to Coverage Program – The First Year in Review Fact Sheet” Georgia Budget and Policy Institute. Jan. 17, 2025 ⤶ ⤶
- “Major Medicaid Eligibility Categories in Tennessee” Tennessee Division of TennCare. Accessed Aug. 7, 2025 ⤶
- ”National Federation of Independent Business v. Sebelius, 567 U.S. 519 (2012)” Justia U.S. Supreme Court. Accessed Dec. 22, 2025 ⤶
- “Early Coverage, Access, Utilization, and Health Effects of the Affordable Care Act Medicaid Expansions: A Quasi-Experimental Study” National Institutes of Health, National Library of Medicine. Apr. 19, 2016 ⤶
- “Wisconsin still losing out from not expanding Medicaid – even under Trump’s big bill” Wisconsin Watch. July 14, 2025 ⤶
- “Georgia didn’t expand Medicaid under Obamacare. Yes, you’re still paying for it” The Atlanta Journal Constitution. Oct. 4, 2024 ⤶
- “Georgia Pathways Current Enrollment” Nov. 30, 2025 ⤶
- “Who could Medicaid reach with expansion in Georgia?” KFF.org. Accessed Dec. 22, 2025 ⤶
- “Medicaid Expansion: Frequently Asked Questions” Center on Budget and Policy Priorities. June 14, 2024 ⤶
- ”Federal and State Share of Medicaid Spending” KFF.org. Accessed Dec. 22, 2025 ⤶
- “Time for Utah to Fully Expand Medicaid” Center on Budget and Policy Priorities. Aug. 1, 2019 ⤶
- “Federal Funding Cuts to Medicaid May Trigger Automatic Loss of Health Coverage for Millions of Residents of Certain States” Georgetown University Center for Children and Families. Nov. 27, 2024 ⤶
- “Enrollment Reports” Virginia Department of Medical Assistance Services. Accessed Aug. 5, 2025 ⤶
- “Current Enrollment” GeorgiaPathways.org. Accessed Dec. 22, 2025 ⤶
- “Medicaid Expansion Enrollment Dashboard” North Carolina Department of Health and Human Services. Accessed Dec. 22, 2025 ⤶
- ”H.R.1 – An act to provide for reconciliation pursuant to title II of H. Con. Res. 14” (Section 71114). Congress.gov. Enacted July 4, 2025 ⤶
- “Where Do the States Stand on Medicaid Expansion?” The Commonwealth Fund. Oct. 17, 2022. And “Why Medicaid Expansion Ballots May Hit a Dead End After a Fleeting Victory in South Dakota” KFF Health News. Dec. 16, 2022 ⤶
- “Why Medicaid Expansion Ballots May Hit a Dead End After a Fleeting Victory in South Dakota” KFF Health News. Dec. 16, 2022 ⤶ ⤶
- “Montana I-185, Extend Medicaid Expansion and Increase Tobacco Taxes Initiative (2018)” BallotPedia. Accessed Aug. 7, 2025 ⤶
- ”Mississippi Medicaid Expansion Initiative (2022)” Ballotpedia. Accessed Dec. 22, 2025 ⤶
- “Medicaid expansion ballot initiative officially halted” Mississippi Today. May 19, 2021 ⤶