What is an out-of-pocket maximum?
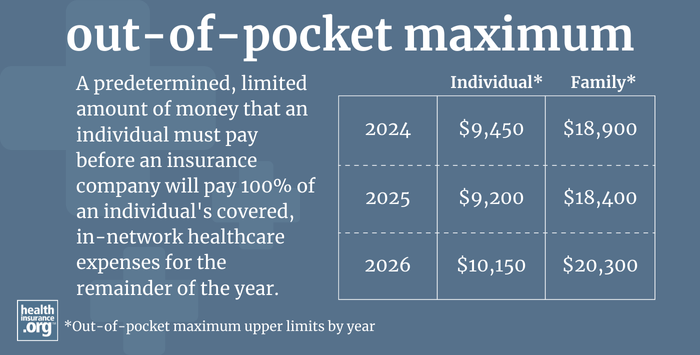
An out-of-pocket maximum is a predetermined, limited amount of money that an individual must pay before an insurance company or (self-insured health plan) will pay 100% of an individual's covered, in-network health care expenses for the remainder of the year.
Health insurance plans can set their own out-of-pocket maximums, but they're constrained by federal regulations that impose an upper limit on how high out-of-pocket costs can be.
- 2025: The upper limits are $9,200 for an individual, and $18,400 for multiple family members on the same plan.1 These are lower than the 2024 limits; 2025 was the first time there had ever been a decrease since out-of-pocket limits debuted in 2014.
- 2026: The limits will increase significantly, to $10,150 and $20,300, respectively.2
It's important to note that the allowable out-of-pocket limits for HSA-qualified high-deductible health plans (HDHPs) are lower, at $8,300 for an individual and $16,600 for a family in 2025.3
Out-of-pocket caps apply to in-network care that's considered an essential health benefit, and only to plans that are not grandfathered or grandmothered or exempt from ACA regulations, as those plans do not have restrictions on their out-of-pocket exposure.
The out-of-pocket limit applies to all other types of private (non-Medicare/Medicaid) health insurance, including individual, small group, large group, and self-insured health plans.
The federal government publishes new guidelines each year that include the highest out-of-pocket maximum that health plans can impose.
(Through 2022, this was published in the annual benefit and payment parameter notice; for 2023 and future years, it's published in guidance that HHS issues no later than January of the prior year; the guidance for 2025 was issued in November 2023,4, and the guidance for 2026 was issued in October 2024.2)
So the highest allowable out-of-pocket maximum changes annually. In 2014, it was just $6,350 for an individual, but by 2026, it will have increased by nearly 60%. Many health plans, however, have out-of-pocket maximums that are well below the highest allowable amounts.
How have out-of-pocket limits changed over the years?
Here are the federally allowed maximum out-of-pocket amounts since they debuted in 2014:
- 2014: $6,350 for an individual; $12,700 for a family
- 2015: $6,600 for an individual; $13,200 for a family.
- 2016: $6,850 for an individual; $13,700 for a family (there was also a requirement starting in 2016 that individual maximum out-of-pocket limits be embedded in family plans).
- 2017: $7,150 for an individual; $14,300 for a family.
- 2018: $7,350 for an individual; $14,700 for a family.
- 2019: $7,900 for an individual; $15,800 for a family
- 2020: $8,150 for an individual; $16,300 for a family.
- 2021: 8,550 for an individual; $17,100 for a family.
- 2022: $8,700 for an individual; $17,400 for a family (note that these are lower than initially proposed; CMS explains the details here)
- 2023: $9,100 for an individual; $18,200 for a family.
- 2024: $9,450 for an individual; $18,900 for a family.
- 2025: $9,200 for an individual; $18,400 for a family.
- 2026: $10,150 for an individual; $20,300 for a family.
How does HHS determine the out-of-pocket maximum?
The out-of-pocket maximum is set each year by HHS. They use a formula that calculates how much the average premium for employer-sponsored health insurance in the preceding year exceeds the average 2013 premium for employer-sponsored health insurance. The out-of-pocket maximum is then based on adjusting the 2014 out-of-pocket maximum by that same percentage growth.
For 2020 and 2021, HHS changed the formula to also include the growth of individual market health insurance premiums since 2013, but switched back to only using employer-sponsored insurance as of 2022.5
So for 2025, HHS looked at how much average employer-sponsored premiums in 2024 ($7,110) exceed average employer-sponsored premiums in 2013 ($4,897). The growth amounted to 45.2%. So that means the maximum out-of-pocket for 2025 is 45.2% higher than the maximum out-of-pocket in 2014. That works out to $9,220, and they round down to the nearest $50, for a 2025 maximum out-of-pocket of $9,200.4
For 2026, the employer-sponsored premium growth from 2013 to 2025 amounted to 60%, because the projected premium for 2025 had grown to $7,833. This pushed the out-of-pocket cap to $10,150 for a single individual — 60% higher than it had been in 2014.2
Are there out-of-pocket caps for Medicare?
There is no out-of-pocket maximum for Original Medicare, which is why most enrollees have supplemental coverage (from an employer-sponsored plan, Medigap, or Medicaid).
Medicare Advantage plans must cap out-of-pocket costs at no more than $9,350 in 2025.6 But that only applies to services that would otherwise be covered under Medicare Part A and Part B. It does not include out-of-pocket costs for prescription drugs covered by the Part D coverage that's integrated with most Advantage plans, nor does it include out-of-pocket costs for extra benefits like dental and vision.
Medicare Part D coverage historically did not have a cap on out-of-pocket costs. However, that changed as of 2024, under the Inflation Reduction Act, when out-of-pocket costs were eliminated once a Part D enrollee reached the catastrophic coverage level. And starting in 2025, a new $2,000 out-of-pocket cap (indexed annually) applies to Part D coverage. This is true regardless of whether the Part D coverage is included in a Medicare Advantage plan or obtained as a stand-alone plan.
Footnotes
- Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2025 Benefit Year. Centers for Medicare and Medicaid Services. Nov. 15, 2023 ⤶
- Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2026 Benefit Year. Centers for Medicare and Medicaid Services. Oct. 8, 2024 ⤶ ⤶ ⤶
- "Revenue Procedure 2024-25" Internal Revenue Service. Accessed Aug. 15, 2024 ⤶
- Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2025 Benefit Year. Centers for Medicare and Medicaid Services. November 2023. ⤶ ⤶
- Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2022 and Pharmacy Benefit Manager Standards. U.S. Department of Health and Human Services. May 2021. ⤶
- "Preliminary Contract Year (CY) 2025 Standards for Part C Benefits, Bid Review and Evaluation" Centers for Medicare & Medicaid Services. Feb. 21, 2024 ⤶
