Medicaid eligibility and enrollment in Arizona

Medicaid expansion enrollment covers more than 613,000 Arizonans; post-pandemic disenrollments began April 1, 2023 in Arizona

Who is eligible for Medicaid in Arizona?
The Medicaid program in Arizona is called the Arizona Health Care Cost Containment System (AHCCCS, which is pronounced “access”). AHCCCS is available to:
- Children birth to 1 year with family income up to 152% of the federal poverty level (FPL)
- Children 1 to 5 years with family income up to 146% of FPL
- Children 6 to 18 with family income up to 138% of FPL
- Children not eligible for Medicaid but with family income up to 205% of FPL are eligible for KidsCare (CHIP)
- Pregnant women with family income up to 161% of FPL (coverage continues for 12 months postpartum)
- Adults under age 65 with family income up to 138% of FPL (Medicaid expansion population)
- Elderly and disabled individuals who meet both income and asset limits
Note that the limits above include a built-in 5% income disregard that’s added to income for MAGI-based Medicaid eligibility (ie, eligibility for children and most adults under 65, but not for those who are elderly or disabled). Also note that Arizona switched to the 2023 FPL numbers on February 1, which was a month or two ahead of many other states (most states implement the updated numbers in March or April).
To check if you qualify for AHCCCS, you can use the Quick Screener on the Health-e-Arizona Plus website. The site houses the online application for medical, food/nutrition, and cash assistance programs, and it connects with the federal health insurance marketplace, HealthCare.gov. You can also see updated income limits for each AHCCCS program here.
Apply for Medicaid in Arizona
Apply online at healthearizonaplus.gov; submit an Application for Benefits by mail (to P.O. Box 19009, Phoenix AZ 85005) or in person; or call 1-855-432-7587 for help applying, or search online for a community assister.
Eligibility: Children 0-1 with family income up to 147% of FPL; age 1-5 with income up to 141% of FPL; 6-18 with income up to 138% of FPL; pregnant women with family income up to 156% of FPL; parents with family income up to 138% of FPL; childless, non-elderly adults with family income up to 138% of FPL; elderly and disabled individuals who have special requirements and meet certain income limits.



ACA’s Medicaid eligibility expansion in Arizona
Arizona accepted federal funding for Medicaid expansion under the leadership of former Governor Jan Brewer, a Republican. Largely as a result of Medicaid expansion, the state’s uninsured rate dropped from 17.1% in 2013 to 10% in 2016. It climbed over the next few years, reaching 11.3% in 2019, but that was in line with the nationwide increase in the uninsured rate under the Trump administration (from 8.6% in 2016 to 9.2% in 2019). And it had dropped slightly, to 10.7%, by 2021.
As of October 2017, there were 398,519 people enrolled in expanded Medicaid in Arizona, according to the state’s waiver proposal requesting additional eligibility rules (details below; the waiver proposal was approved in January 2019). Arizona’s Medicaid expansion enrollment grew significantly during the COVID pandemic (as was the case nationwide), and 613,163 Arizona residents were enrolled in Medicaid expansion coverage as of September 2023 (this includes 530,316 with income below the poverty level, plus 82,847 with income between the poverty level and 138% of the poverty level). Total Medicaid expansion enrollment in Arizona is down from nearly 700,000 before post-pandemic disenrollments resumed in April).
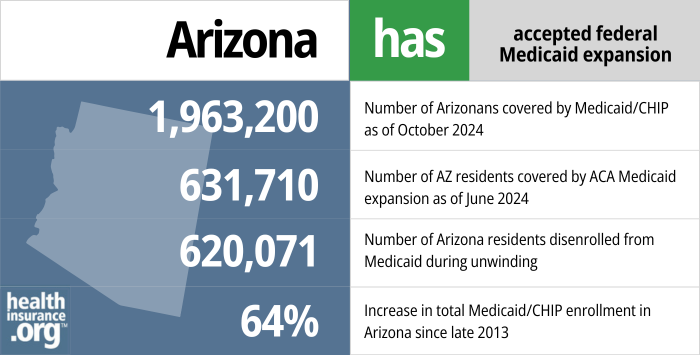
- 1,963,200 – Number of Arizonans covered by Medicaid/CHIP as of October 20241
- 631,710 – Number of AZ residents covered by ACA Medicaid expansion as of June 20242
- 620,071 – Number of Arizona residents disenrolled from Medicaid during unwinding3
- 64% – Increase in total Medicaid/CHIP enrollment in Arizona since late 20134
Explore our other comprehensive guides to coverage in Arizona

This guide was created to help you better understand the Arizona Marketplace and pick the right health plan for you and your family. For many, an Affordable Care Act (ACA) Marketplace plan – also called an Obamacare plan – may be a good choice.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Arizona.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Arizona as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Arizona Medicaid eligibility and enrollment
How do I enroll in Medicaid in Arizona?
The quickest way to apply for AHCCCS is online at www.healthearizonaplus.gov. This works for anyone eligible for AHCCCS, including those who are also eligible for Medicare and thus have both income and asset limits for eligibility.
You can also call 1(855)-HEA-PLUS (1-855-432-7587), between 8 a.m. and 5 p.m., Monday to Friday. (The phone number for AZ Relay Service for the hearing impaired is 1-800-842-6520)
If you are 65+, blind, or disabled, you have the option to print an Application for Benefits form, complete it, and mail it to:
AHCCCS Medical Assistance Specialty Programs (MA-SP)
801 E Jefferson St
Phoenix AZ 85034
How does Medicaid provide financial assistance to Medicare beneficiaries in Arizona?
Many Medicare beneficiaries receive help through Medicaid with paying for Medicare’s premiums, programs that lower prescription drug costs, and services Medicare doesn’t cover — such as long-term care.
Our guide to financial assistance for Arizona Medicare enrollees explains these benefits, including Medicare Savings Programs, long-term care benefits, Extra Help, and eligibility guidelines for assistance.
How is Arizona handling Medicaid post-pandemic Medicaid renewals?
Medicaid disenrollments were paused nationwide from March 2020 through March 2023, due to the COVID pandemic. But that’s no longer the case, and states are now disenrolling people who are no longer eligible for Medicaid. States have a 12-month “unwinding” period to redetermine eligibility for everyone enrolled in Medicaid and disenroll those who aren’t eligible or who fail to respond to renewal notices.
Arizona began the eligibility redetermination process in February 2023, allowing disenrollments (related to the first round of renewals that were processed) to resume on April 1, 2023 (most states waited until March or April to begin the process, and thus had their initial disenrollments later in 2023). AHCCCS data indicate that enrollment in Arizona dropped by more than 289,000 people between April and August 2023, and total enrollment was under 2.3 million people by September. However, more than 800,000 enrollees’ coverage had been renewed between April and August, as they still met the eligibility guidelines (and completed renewal paperwork as necessary).
Arizona Medicaid (AHCCCS, or Arizona Health Care Cost Containment System) had roughly 500,000 enrollees who had either not responded to renewal notices during the pandemic, or who were likely “factually ineligible,” which means that Arizona Medicaid had received information indicating that the person was no longer eligible (for example, due to aging out of an age-based eligibility category, or an income increase). These people were not disenrolled during the pandemic, due to the federal rules, but they are being disenrolled now.
Arizona’s Medicaid website includes an overview of the state’s process of returning to regular renewals and disenrollments. The state continued to process renewals as possible during the pandemic (ie, automatically, or if the enrollee responded to the renewal notices that the state continued to send out), thus minimizing backlog.
But for the 500,000 people who were enrolled under the COVID-related continuous coverage rules (ie, the state either knew they were no longer eligible, or hadn’t received information verifying that they were eligible), eligibility redeterminations are necessary, with ineligible people being disenrolled as of their renewal date.
Arizona has been working through those 500,000 enrollees by prioritizing people who were factually ineligible and then working on renewals for people who did not respond to the state’s requests for renewal information during the continuous coverage period. For both groups, the state began with the files that had been held open the longest, and worked forward to more recent cases (this is the “hybrid” option that CMS detailed in its summary of how states could address the unwinding of the Medicaid continuous coverage requirement).
Arizona has also enacted legislation that requires the state to complete eligibility redeterminations for this population by December 31, 2023. This applies to people who are factually ineligible based on information the state has on file, or whose eligibility has not been redetermined since December 2022. Under federal rules, they have a full 12 months to initiate eligibility redeterminations for the entire AHCCCS population (plus two additional months to complete the process), but the state’s new law ensures that people who are factually ineligible or whose cases have been pended since 2022 or earlier will have their eligibility redetermined earlier in the unwinding process.
The legislation does still allow Arizona to comply with the federal recommendation that states process renewals for no more than one-ninth of their Medicaid population each month during the unwinding period. Arkansas is using a somewhat similar approach, and so is Oklahoma.
It’s noteworthy that Arizona has said that they’re able to process roughly three-quarters of renewals automatically, without the enrollee having to provide any additional information. This is significantly higher than the automatic (ex parte) renewal rate in most states. Arizona is also among the minority of states that were in compliance with federal rules that require eligibility determinations to be conducted on an individual (rather than household) level. This ensures, for example, that children who qualify for automatic renewal don’t get disenrolled just because their parents are no longer eligible or failed to respond to a renewal packet.
Legislation impacting Arizona Medicaid
Arizona lawmakers have pushed for changes to Medicaid eligibility and benefits since 2015
In the 2015 legislative session, Arizona lawmakers passed Senate Bill 1092, which made an effort to dial back the state’s expansion of Medicaid. SB1092 requires the state to submit an 1115 waiver request to CMS every year, asking for approval for new Medicaid eligibility guidelines.
(H.B.2228, which was enacted in 2018, calls for the exemption of Native Americans from any new Medicaid eligibility rules that are implemented as a result of Arizona’s waiver process; the Trump administration’s approval of Arizona’s Medicaid waiver in 2019 includes an exemption from the new rules for Native Americans, but only if they’re enrolled citizens of their tribes.)
Lawmakers wanted the new eligibility rules to include a five-year limit on Medicaid coverage for able-bodied adults, along with a provision requiring enrollees to be working or involved in job training or school. In August 2015, Governor Doug Ducey unveiled his proposals for Arizona’s first Medicaid waiver proposal, including a work requirement and the five-year lifetime limit on Medicaid coverage for able-bodied adults.
The idea was that Medicaid would remain a solid safety net for children and disabled adults, but that it would become a more temporary program for able-bodied adults. Ducey’s waiver proposal also included a requirement that enrollees pay increased premiums and cost-sharing and establish health savings accounts, and participate in various wellness programs like flu shots and glucose screening.
Many advocates for low-income Arizona residents were worried that Ducey’s proposal would be a setback, chipping away at the hard-won gains the state has made in reducing the uninsured rate.
Obama administration approved Arizona’s new Medicaid waiver, but with several provisions removed
The state continued to work with CMS to come to an agreement on a new waiver, and Arizona published a revised version of their proposed Medicaid modernization waiver in July 2016. CMS approved Arizona’s waiver proposal, but eliminated the most conservative aspects of it. The new waiver runs through September 2022 (including a one-year extension so that CMS and Arizona could continue negotiations over a longer-term extension), and includes the following provisions:
- A new AHCCCS CARE program for enrollees with income above the poverty level (between 100% and 138% of the poverty level, as those individuals are eligible for Medicaid under the ACA’s expansion). The program requires modest contributions to a health savings account, but the premiums can be deferred for six months if members complete various wellness and preventive care requirements.
- A job search program that’s offered but not mandatory (as described below, the Trump administration allowed the state to change this to a mandatory community engagement requirement, but the state opted to indefinitely postpone implementation due to the uncertain legal status of work requirements in other states, and the Biden administration officially rescinded approval for Arizona’s work requirement in June 2021).
The Obama administration CMS declined several provisions of the original waiver proposal, including the five-year limit on AHCCCS benefits for able-bodied adults, and the work/job search requirement — it was changed to a program in which beneficiaries are automatically enrolled, but AHCCCS benefits are not eliminated for those who don’t actively participate.
CMS also refused to allow Arizona to charge premiums for beneficiaries with income under the poverty level, lock people out of re-enrolling in Medicaid for six months if they don’t pay their premium contributions to the health savings account, or charge fees for missed medical appointments.
All of the details about Arizona’s 1115 waiver proposal and the response from CMS are available here.
Trump administration approved Arizona’s work requirement proposal with a 2020 effective date; Arizona indefinitely postponed implementation amid legal uncertainty, and the Biden administration withdrew approval in 2021
The Trump administration clarified in early 2018 that they were open to work requirements, and approved them for several states. In late 2017, Arizona submitted their AHCCCS Works waiver proposal as an amendment to the already-approved waiver the Obama administration had granted in 2016 (an additional amendment, submitted in April 2018, proposed eliminating retroactive coverage).
The proposal was partially approved in January 2019, allowing Arizona to implement the following changes:
- Work requirement (which would have been effective no earlier than January 2020): If this requirement had been implemented, Medicaid expansion enrollees between the ages of 19 and 49 would have had to work (or participate in other “qualifying community engagement activities”) at least 80 hours per month, and report their compliance to the state. Non-compliant enrollees — including those who are working but not reporting their work hours to the state — would have had a three-month grace period, after which they would have lost their Medicaid coverage for two months. Exemptions would have applied for various groups, including pregnant women, homeless people, full-time students, victims of domestic violence, and parents caring for minor children.
- In September 2019, Arizona officials announced that the work requirement would not take effect until the fall of 2020, and would initially only be implemented in urban areas of the state (Maricopa, Pima, and Yuma counties), with implementation in some rural areas (Apache, Gila, Graham, Greenlee, La Paz, and Navajo counties) potentially delayed until 2022.
- In October 2019, Arizona officials sent a letter to CMS, notifying the federal government that the state has decided to postpone implementation of the work requirement “until further notice.” The state’s decision to suspend the work requirement was based on “the evolving national landscape concerning Medicaid community engagement programs” and the legal uncertainty these programs are facing in other states. Instead of moving forward with implementation of a program that seems increasingly likely to be judicially overturned, Arizona decided to shelve the idea for the time being.
- In March 2020, the Families First Coronavirus Response Act provided additional federal Medicaid funding to states, but only if they didn’t disenroll anyone from their Medicaid rolls for the duration of the COVID emergency period. That effectively shut down the concept of Medicaid work requirements for the duration of the COVID pandemic.
- In June 2021, the Biden administration notified Arizona that the Medicaid work requirement approval was being withdrawn. So a work requirement will not take effect in Arizona after the COVID public health emergency ends.
- Waiver of retroactive eligibility, meaning that coverage would take effect the month the person applies, instead of taking effect up to three months prior to the month the person applies. The waiver of retroactive eligibility won’t apply to pregnant and postpartum women, or to children under the age of 19.
But the Trump administration did not approve all of Arizona’s proposals. Notably:
- HHS did not approve the state’s proposed five-year limit on Medicaid coverage for expansion enrollees who don’t comply with the work requirement.
- HHS also did not approve the state’s request to have the federal government pay for the bulk of the cost of implementing the work requirement. The federal government pays most of the cost of providing medical care to Medicaid expansion enrollees (93% in 2019, dropping to 90% in 2020 and future years), and Arizona wanted the federal government to use that same funding rate to help the state cover the cost of setting up the system to administer the work requirement. HHS declined.
Arizona Medicaid history
Arizona was the last state to implement a traditional Medicaid program, establishing AHCCCS in October 1982. Arizona’s Medicaid program has operated for more than 25 years under a Section 1115 waiver that allows the state to use capitated managed care. About 84% of Arizona’s Medicaid beneficiaries receive services through managed care arrangements (as of 2023, there are eight managed care plans from which AHCCCS members can choose, although plan availability varies by location). Medicaid managed care helps states provide access to health care providers, improve quality of care, and control financial risk.
Arizona froze enrollment in KidsCare—its version of the Children’s Health Insurance Program— in 2010, and discontinued KidsCare at the end of January 2014 due to lack of funding. For more than two years, Arizona was the only state that didn’t have CHIP. But in July 2016, CMS approved Arizona’s proposal to re-open CHIP. Enrollment began July 26, and coverage took effect as early as September 1, 2016. The state expected 30,000 to 40,000 children to be newly eligible for CHIP. (As of January 2023, there were a total of 72,623 children enrolled in KidsCare.)
Medicaid expansion under the Affordable Care Act was signed into law in Arizona in July 2013. Arizona was one of the first states led by a Republican governor to sign on to expansion.
In February 2017, the Arizona Court of Appeals heard a case, brought by Republican lawmakers, challenging whether the state’s assessment on hospitals ($265 million a year, used to fund the state’s portion of Medicaid expansion costs) was legal. But in March 2017, the appeals court rejected the lawsuit, ruling that the assessment was legal and that Medicaid expansion could continue.
In December 2014, CMS approved a new 1115 waiver for Arizona’s Medicaid program, although they declined to approve some aspects of the proposal, including a proposed $200 fee for non-emergency use of an emergency room for Medicaid enrollees with income above the poverty level.
In September 2016, CMS approved another waiver proposal, but did not agree to some of the state’s requests, including a work requirement and lifetime limit on Medicaid eligibility. The waiver created a new AHCCCS CARE program for enrollees with income above the poverty level, with enrollees required to make modest contributions to a health savings account. There was also a voluntary job search program.
Arizona submitted a new waiver proposal to the Trump administration, which called for a work requirement and a five-year limit on Medicaid eligibility for the Medicaid expansion population if they failed to comply with the work requirement. The Trump administration approved the work requirement (although as noted above, Arizona indefinitely postponed implementation and the work requirement approval was rescinded by the Biden administration), and began allowing Arizona to eliminate retroactive Medicaid coverage for most enrollees. But they rejected the five-year limit on Medicaid expansion coverage, and declined to pay the bulk of the cost for the state to administer the work requirement.
The American Rescue Plan provided funding for states to offer 12 months of postpartum Medicaid coverage, instead of terminating a mother’s coverage 60 days after the baby is born. AHCCCS announced in September 2022 that they would implement this option. Under the American Rescue Plan, funding for this was only provided for five years, but the Consolidated Appropriations Act, 2023, makes this option permanent for states.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, data.medicaid.gov, Accessed February 2025 ⤶
- “Medicaid Enrollment and Unwinding Tracker“, KFF.org, Accessed March 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment” , kff.org, Accessed January 2025 ⤶

