Medicaid eligibility and enrollment in Idaho

Idaho House has passed legislation that would make significant changes to Medicaid expansion in the state

Who is eligible for Idaho Medicaid?
Compared to many other states, Idaho has a more restrictive Medicaid program. Idaho Medicaid eligibility levels are as follows, including a federally-required 5% income disregard):
- Children ages 0-5 qualify with family income up to 147% of the federal poverty level (FPL)
- Children ages 6-18 qualify with family income up to 138% of the FPL
- Pregnant women qualify with family income up to 138% of the FPL (coverage ends for the mother 60 days after the birth; Idaho is not among the majority of the states where postpartum Medicaid coverage has been extended to 12 months; legislation to extend postpartum Medicaid coverage failed in Idaho in 2023)
- Low-income adults (under age 65) with income up to 138% of FPL, due to Medicaid expansion under the ACA.
- Children qualify for CHIP (Children’s Health Insurance Program) with family income up to 190% of the FPL.
See the Idaho Medicaid website for eligibility criteria for individuals who are aged or disabled; note that for these populations, there are both income and asset limits for Medicaid eligibility.
Apply for Medicaid in Idaho
Complete an application online or call 1-877-456-1233 for assistance.
Eligibility: Children ages 0-5 with family income up to 142% of FPL. Children ages 6-18, pregnant women, and adults up to age 64 with family income up to 138% of FPL. See additional eligibility criteria for individuals who are aged or disabled.



Has Idaho expanded Medicaid under the ACA?
Yes, Idaho has accepted federal funding to expand Medicaid as called for in the ACA. Idaho’s Medicaid expansion took effect in January 2020, after voters approved Proposition 2 by a wide margin in the 2018 election. Medicaid expansion in Idaho was ultimately implemented without modifications, after state lawmakers unsuccessfully tried to make various changes to the way the expansion would work. This is discussed in more detail below.
By early 2023, about 145,000 people were enrolled under Medicaid expansion in Idaho.1 But that had dropped to 93,337 by mid-2024,2 due to the “unwinding” of pandemic-related continuous coverage rules (discussed below). It had dropped a little more, to just over 90,000 people, by the end of 2024.3
In January 2025, lawmakers in Idaho introduced legislation that would repeal Medicaid expansion in the state, starting in July 2025, although it had not advanced by later March.4
However, another bill, which calls for significant changes to the program, passed in the Idaho House in February 2025 and was sent to the Senate for consideration. That bill, HB138, calls for the state to obtain waivers that would allow a work requirement as well as an option for people with income between 100% and 138% of the federal poverty level to choose either Medicaid or a Marketplace premium subsidy. The legislation also calls for Medicaid expansion enrollment to be capped at no more than 50,000 people, as well as a “trigger law” that would end Medicaid expansion in Idaho if federal funding drops below 90% (the measure had not yet advanced in the Idaho Senate by late March).5
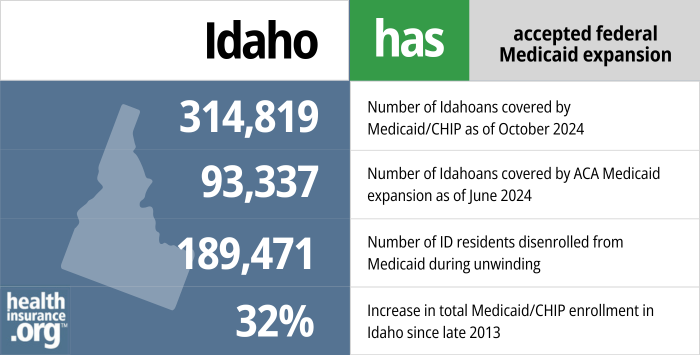
- 314,819 – Number of Idahoans covered by Medicaid/CHIP as of October 20246
- 93,337– Number of Idahoans covered by ACA Medicaid expansion as of June 20247
- 189,471 – Number of ID residents disenrolled from Medicaid during the post-pandemic “unwinding” process8
- 32% – Increase in total Medicaid/CHIP enrollment in Idaho since late 20139
Explore our other comprehensive guides to coverage in Idaho

This Idaho health insurance guide is designed to help you understand the health coverage options and possible financial assistance available to you and your family in Idaho.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Idaho.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Idaho as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Idaho Medicaid eligibility and enrollment
How do I apply for Idaho Medicaid?
You can apply for Idaho Medicaid on-line, in person, over the phone, or by submitting a paper application.
- Online: Visit the idalink portal or the Your Health Idaho website.
- In Person: Visit a Health & Welfare office.
- By Phone: Call 1-877-456-1233
- Paper application: Print and complete the application form, and then return it by fax (1-866-434-8278) or mail (Self Reliance Programs; PO Box 83720; Boise, ID 83720-0026)
How does Medicaid provide assistance to Medicare beneficiaries in Idaho?
Many Medicare beneficiaries also receive assistance through Medicaid. This can include help with Medicare premiums, cost sharing (i.e., deductibles, co-pays and coinsurance), and long-term care expenses.
Our guide to financial assistance for Medicare beneficiaries in Idaho details these programs, including Extra Help, long-term care Medicaid, and eligibility guidelines for assistance.
How did Idaho handle Medicaid renewals after the pandemic?
During the COVID pandemic, states received additional federal Medicaid funding, on the condition that they not disenroll anyone from Medicaid. States were able to conduct regular Medicaid renewals/eligibility redeterminations, but were not allowed to disenroll people who didn’t respond to renewal requests or who were determined to no longer be eligible. But the federal continuous coverage rule for Medicaid ended on March 31, 2023, so states could start disenrolling people as early as April 1, 2023.
Idaho opted to begin the process on the earliest timeframe that HHS allowed, so they initiated renewals on February 1, 2023, and disenrollments began April 1.
By early September 2023, Idaho officials announced that they had completed eligibility determinations for all enrollees whose eligiblity status had not been current as of the spring. Out of 153,000 eligibility re-checks, the state had determined that about 32,000 people were still eligible (their coverage was renewed) while about 121,000 were no longer eligible or did not respond to renewal notices, and their coverage was terminated.
Idaho Medicaid continued to conduct regular eligibility redeterminations throughout the pandemic. State officials noted in early 2023 that they had about 450,000 people enrolled in Medicaid, and about 300,000 of them were current on their renewals — meaning that the state had processed an application or renewal within the last 12 months and confirmed that the person was still eligible for coverage.
But nearly 154,000 people were on what Idaho referred to as “Medicaid protection,” which means that they were either no longer eligible or hadn’t responded to a renewal notification, but their coverage had remained in force due to the pandemic-related rules. Idaho processed renewals for these 154,000 people first, starting in February 2023, and they met their goal of processing all of them by the end of August.
Idaho prioritized eligibility redeterminations for the people who were on Medicaid protection, and then completed eligibility redeterminations for the rest of their enrollees. By February 2024, a total of more than 189,000 people had been disenrolled from Idaho Medicaid.8
People who were determined ineligible to keep their Medicaid were referred to Your Health Idaho (the state-run exchange) to secure new coverage. They could also transition to an employer’s plan if available, or to Medicare if they were eligible for that program.
How many people are enrolled in Idaho Medicaid?
As of October 2024, there were 314,819 people enrolled in Medicaid and CHIP in Idaho.6 This was about 32% higher than enrollment had been in 2013,9 with the growth due largely to Medicaid expansion that took effect in the state in 2020.
Enrollment had been much higher in early 2023, but as described above, it declined significantly during the “unwinding” of the pandemic-related continuous coverage rule that was in effect from March 2020 to March 2023.
Idaho Medicaid history and details
Does Idaho have a Medicaid work requirement?
Idaho does not have a Medicaid work requirement. The state enacted S.1204 in 2019, which directed Idaho officials to seek federal permission to implement a Medicaid work requirement. Later in 2019, Idaho submitted a waiver proposal to CMS for a Medicaid work requirement, but it was not approved by the first Trump administration or by the Biden administration.
Legislation that would create a work requirement (pending federal approval) passed the Idaho House in February 2025, although it had not advanced in the Senate by late March 2025.5
Idaho lawmakers’ proposed modifications for Medicaid expansion
Idaho HB138, which passed in the state House in February 2025 but had not advanced in the Senate by late March, calls for substantial changes to Medicaid expansion in Idaho.5
the legislation would direct Idaho to obtain federal waivers to:
- Create a work requirement for Medicaid expansion enrollees.
- Create the option for people with income between 100% and 138% of the federal poverty level to choose either Medicaid or a Marketplace premium subsidy (no state has ever received federal approval for something like this; as noted below, this was something that Idaho unsuccessfully sought approval for under the first Trump administration).
HB138 also calls for Medicaid expansion enrollment to be capped at no more than 50,000 people (there were more than 90,000 enrollees in late 2024).3
The legislation also includes a “trigger law” that would end Medicaid expansion in Idaho if federal funding drops below 90%.
In addition, lawmakers in Idaho introduced legislation in early 2025 that calls for the repeal of Medicaid expansion by mid-2025, although its future is uncertain and it would be at odds with the expansion ballot measure that Idaho voters approved in 2018.4
Proposition 2, which Idaho voters approved by a wide margin in the 2018 election, directed the state to expand Medicaid as called for in the ACA. The text of the ballot initiative (see page 10 of the voter guide) called for the state to submit an expansion plan to the federal government within 90 days, and to implement to provisions of the proposition “as soon as practicable.”
But Idaho lawmakers took a round-about approach to implement the ballot initiative. Early in the 2019 legislative session, some of the state’s conservative lawmakers began working to draft legislation that would call for various restrictions on Medicaid expansion, including things like work requirements, copays, premiums, or lifetime limits on coverage. Rep. John VanderWoude, R-Nampa, noted in early 2019 that although the details were still being sorted out at that point, “if we do nothing, then we’re left with full-blown Medicaid expansion.”
Idaho S.1204 was designed to move the state forward with expansion, but with various additional restrictions — most notably, a work requirement — despite the fact that 61% of Idaho’s voters approved a “clean” (i.e., not modified) expansion of Medicaid in the November 2018 election. And a poll conducted in February 2019 indicated that nearly three-quarters of the state’s residents wanted lawmakers to implement Medicaid expansion as called for in Proposition 2, while just 17% wanted lawmakers to make changes to how expansion would be implemented.
S.1204 passed both chambers of the Idaho legislature and was signed into law by Governor Brad Little on April 9, 2019. The legislation called for some notable deviations from a “clean” Medicaid expansion, some of which require approval from CMS.
Idaho submitted a waiver proposal to CMS for a Medicaid work requirement, but it was never approved. The Biden administration has revoked all of the already-approved work requirement waivers in other states, and has noted that work requirements run counter to Medicaid’s mission, which is simply to provide health coverage to people in need. In addition, Idaho’s “coverage choice” proposal was rejected by CMS under the Trump administration. Here’s an overview of what Idaho was trying to implement:
- Work requirement: A work/community engagement requirement, under which able-bodied enrollees aged 19-59 would have to work/attend school, etc. for at least 20 hours a week in order to maintain Medicaid eligibility. CMS approved Medicaid work requirements for several states under the Trump administration, but they faced numerous legal challenges and became essentially unworkable during the COVID pandemic. And they were all revoked by the Biden administration in 2021.
Idaho submitted a proposal to CMS in October 2019, after gathering public feedback on the proposal (it’s notable that the majority of the people who provided public testimony were opposed to the work requirement). The proposal is still under review in 2023, but very unlikely to be approved or implemented under the Biden administration. - “Coverage choice”: A provision allowing people with income between 100% and 138% of the poverty level to continue to receive premium subsidies to buy coverage in the Idaho exchange (as they had been able to do since 2014), or to switch to expanded Medicaid. In his approval letter for S.1204, Governor Little noted that the negotiations with CMS over this provision would be “challenging,” but expressed his confidence that Idaho regulators would be able to work out a solution with CMS.
In July 2019, the state submitted a waiver proposal to seek federal approval for this. But CMS responded in August, noting that the waiver proposal incomplete, and that “even if the application were revised to include the correct elements, Idaho’s application would not be approvable because it could not demonstrate compliance with the statutory guardrails, in particular, the deficit neutrality guardrail.” (1332 waivers can only be approved if they won’t increase the federal deficit; it’s noteworthy that it’s cheaper for a state to keep the 100-138% of poverty level population in the exchange, since premium subsidies are funded entirely by the federal government, whereas Medicaid expansion is funded with a 90/10 split, with the state paying 10% of the cost.) Idaho’s Governor and legislative leaders indicated that they were surprised by the CMS decision. - A health risk assessment that includes questions about substance use disorders (the legislation notes that the data would be used to refer enrollees to substance abuse treatment; there is nothing in the legislation that would restrict access to Medicaid coverage based on answers to the health risk assessment).
- Managed care: The use of Medicaid managed care for all Medicaid expansion enrollees. This has been a fairly standard approach used by most states.
S.1204 noted that Medicaid expansion wouldn’t be delayed if there was a delay in CMS approval of the state’s proposal or if CMS failed to approve some portions of what the state proposed. So Medicaid expansion in Idaho still took effect January 1, 2020 (enrollment began November 1, 2019), despite the fact that the state had failed to gain federal approval for the “coverage choice” proposal and the work requirement waiver proposal was still pending federal approval (indeed, it’s still pending federal approval as of 2023).
BYU-Idaho reversed course, continued to accept Medicaid as an alternative to the school’s non-ACA-compliant student health plan
In late 2019, after significant student backlash and public attention, BYU-Idaho retracted its new rule that would have prevented students with Medicaid from waiving coverage under the school’s student health plan. Students with Medicaid, including those newly eligible under Idaho’s Medicaid expansion, continue to be able to waive the school’s health plan and rely on Medicaid instead. The school issued a statement and sent a campus-wide email in which they “apologize for the turmoil” caused by their earlier decision.
Soon after enrollment in Idaho’s Medicaid expansion began in November 2019, BYU-Idaho had revised its rules for waiving the school’s student health plan. When we contacted the school at that point, a representative confirmed that as of the spring 2020 semester, Medicaid (from Idaho or any other state) would no longer be considered coverage that will allow a student to waive enrollment in BYU-Idaho’s student health plan.
Many schools, BYU-Idaho among them, require students to maintain health insurance. Previously, the waiver form indicated that students with Idaho Medicaid could waive the student health plan, but that Medicaid coverage from another state could not be substituted for the school’s student health plan.
Somewhat ironically, BYU’s student health plan is not considered minimum essential coverage under the ACA, while Medicaid is. BYU-Idaho’s student health plan is self-insured, and while nearly all student health plans are regulated by the ACA, those regulations don’t apply to the small minority of student health plans that are self-insured.
More than 12,000 people signed a petition asking BYU-Idaho to reverse course, and the story quickly garnered national attention in the days before school officials decided to reverse course and allow students to continue to use Medicaid as their health coverage. The school had put out a statement indicating that they were concerned that students on Medicaid would overwhelm the resources of the local medical providers, but doctors and medical facilities in the area had indicated they had no such concerns.
And although most students were able to continue to go to school at BYU-Idaho with their health coverage uninterrupted, the uncertainty created by the university’s initial decision caused some students to change their plans for the spring 2020 semester.
Medicaid expansion upheld by the Idaho Supreme Court
After voters in Idaho overwhelmingly approved Proposition 2, the state added a new section to its insurance statutes. Section 56-267 codifies Medicaid expansion into Idaho law, under the terms of the ballot initiative.
But soon thereafter, local GOP leader Brent Regan filed a lawsuit, asserting that Section 56-267 was unconstitutional. Regan is the Chairman of the Kootenai County Republican Central Committee, and also serves as Board Chair for the Idaho Freedom Foundation. Regan’s lawsuit was centered around his belief that Section 56-267 gives too much power to the executive branch, and relies on federal rules that could be changed in the future (the statute says that the state’s Medicaid expansion should apply “in accordance with sections 1902(a)(10)(A)(i)(VIII) and 1902(e)(14) of the Social Security Act.” Those sections describe who is eligible for Medicaid expansion under the ACA, including income limits and how income is calculated).
Opponents of Regan’s lawsuit note that the only power granted to the Department of Health and Welfare is related to implementation of the law — not making or changing anything about Idaho law.
The Idaho Supreme Court heard oral arguments in the case on January 29, 2019, and issued a ruling the following week (summary of the ruling is available here). The Court ruled that Section 56-267 is not unconstitutional and does not delegate excessive authority to the Department of Health and Welfare or the federal government. Numerous Idaho laws reference federal statute, and Section 56-267 is no different. The Court also noted that Idaho case law clarifies that such references to federal policy apply to the federal policy at the time the state statute is adopted.
Idaho’s path to Medicaid expansion
For years, more than 75% of Idaho residents had been in favor of Idaho lawmakers coming up with a solution to allow the people in the Medicaid coverage gap to gain access to comprehensive health insurance. The Idaho Hospital Association and the Idaho Medical Association also supported the expansion of Medicaid, noting that Medicaid expansion helps rural hospitals remain open, and ensures that low-income residents have realistic access to medical care.
Idaho’s Medicaid Redesign Group in November 2014 recommended the Healthy Idaho Plan. The workgroup, formed by then-Gov. Otter, repeatedly expressed support for Medicaid expansion. The Healthy Idaho Plan would have extended Medicaid eligibility to adults up to 100% of the federal poverty level (FPL) and provided subsidies to help those between 100 and 138% of FPL to purchase coverage through Your Health Idaho. Proponents said that implementing the Healthy Idaho Plan would have saved the state $173 million over ten years by eliminating the Catastrophic Health Care Cost Program. The CAT program, as it is commonly called, covered some health care costs incurred by the very poor. The CAT program was funded through the state general fund and county property taxes.
In his 2015 State of the State address, Gov. Otter asked state legislators to consider the recommendations from the Medicaid Redesign Group, but he stopped short of endorsing it. Republican leaders said they would consider the option, but they remained skeptical of Medicaid expansion. County Commissioners throughout the state voted to support the Healthy Idaho Plan in September 2015.
Your Health Idaho (the state-run exchange) said that 54,000 people applied for coverage through the exchange in 2014 and were unable to get subsidies because their income was below the poverty level. For the population in the coverage gap, health insurance was essentially unavailable prior to Medicaid expansion, as their only option would have been to pay full price for a private plan — clearly not feasible for people with income below the poverty level.
Lawmakers also considered much less robust solutions in 2016 (the Idaho Primary Care Access Program) and in 2017 (the Health Care Assistance Program), but neither solution was enacted.
In February 2016, the Senate Health and Welfare Committee heard public testimony for the first time regarding Medicaid expansion. But no agreements were reached in Idaho regarding health coverage for the state’s lowest-income residents.
During the 2016 legislative session, lawmakers considered three bills related to Medicaid expansion and care for people in the coverage gap, but none made it out of committee:
- S1204 would have expanded Medicaid as called for in the ACA, providing coverage to everyone with household incomes up to 138 percent of the poverty level.
- S1205 would have implemented a modified version of Medicaid expansion (Healthy Idaho – see details below), which was recommended by Otter’s work group. S1205 would require a waiver from HHS, but the basics have already been pre-approved by HHS.
- H484 would have implemented Governor Otter’s Primary Care Access Program.
In March 2016, in response to fellow Senators’ failure to even consider Medicaid expansion during the 2016 session, Senator Dan Schmidt (D, Moscow), announced that he would relinquish the health insurance benefits he receives as a member of the Idaho legislature. Sen. Schmidt is a family physician, and has worked for three years to expand Medicaid in Idaho. He expressed his disappointment that lawmakers once again failed to come up with a solution for the people in the coverage gap in Idaho. Schmidt noted that: “My state-funded health insurance is quite expensive for the taxpayer, yet the coverage for the gap population would require no tax increase—indeed, even reduce some costs to the taxpayer. But I receive this benefit, and they don’t. It’s not fair, and my wife and I agree we should not participate in this unfairness.”
After the legislature’s failure to address the Medicaid coverage gap in 2016, House Majority Leader Scott Bedke announced that he would appoint a bipartisan committee to address the issue, and committed to addressing the Medicaid coverage gap during the 2017 legislative session. The ten-member committee began meeting during the summer of 2016, and although they received overwhelming public support for Medicaid expansion, at least four of the members were still expressing opposition to the ACA’s Medicaid expansion as of August 2016.
In February 2017, lawmakers introduced H.160, which would have created the Health Care Assistance Program. A similar bill, S.1142, was introduced in the Senate. Neither bill advanced out of committee, however, and the legislative session ended on March 29.
Medicaid expansion legislation was introduced once again in the Idaho legislature in 2018, but it died in committee and never reached a vote. But expansion advocates bypassed the legislature altogether and took the issue to the state’s voters. Proponents of Medicaid expansion gathered enough signatures to get Proposition 2 on the ballot in Idaho in November 2018, allowing voters in the state to decide whether to expand Medicaid. And voters approved it by a wide margin.
Otter supported Proposition 2, but he was term-limited, and the state’s lieutenant governor, Republican Brad Little, won the gubernatorial election in November 2018. Although Little’s victory speech noted that he was “look[ing] forward to working with President Trump to continue to allow Idahoans to be the masters of their own destiny,” Little had said previously that he would respect the will of the voters on the Medicaid ballot initiative. And the voter-approved Medicaid expansion measure was ultimately implemented in late 2019, with coverage effective in 2020.
Idaho Medicaid history
Idaho implemented its Medicaid program in July 1966, one year after the program was authorized at the federal level.
The Idaho Department of Health & Welfare oversees the Idaho Medicaid program. A department webpage details three Medicaid benefit plans for adults: a Basic Plan to provide medical services for low-income working-age adults; an Enhanced Plan that provides medical services, developmental disability services, enhanced mental health coverage, and long-term care services for individuals with special needs; and a Coordinated Plan that provides medical services to individuals who are dually eligible for Medicare and Medicaid.
Prior to 2020, there were an estimated 78,000 Idaho residents in the coverage gap — ineligible for subsidies in the exchange and also ineligible for Medicaid. But these individuals — in addition to people with income from 100% to 138% of the poverty level who had previously been eligible for subsidies in the exchange — are now eligible for Medicaid in Idaho.
Medicaid expansion took effect in 2020 in Idaho. The state had initially expected total enrollment in expanded Medicaid to eventually reach 91,000 people, but that was before the COVID pandemic. The pandemic increased Medicaid enrollment nationwide, due to the widespread job losses and the fact that the additional federal Medicaid funding (in the Families First Coronavirus Response Act) was contingent on states not disenrolling anyone from their Medicaid rolls between March 2020 and March 2023 (as discussed in more detail above, disenrollments resumed April 1, 2023, and roughly 189,000 people were disenrolled from Idaho Medicaid during the year-long “unwinding” process).
By the end of 2024, about 90,000 people were covered by Idaho Medicaid expansion3 — very much in line with what the state had initially predicted.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- ”An FAQ about Medicaid Expansion and continuous enrollment” Idaho Department of Health & Welfare. Jan. 27, 2023 ⤶
- ”Medicaid Enrollment – New Adult Group” Medicaid.gov. Data through June 2024. Accessed Jan. 30, 2025 ⤶
- ”Bill to repeal Medicaid expansion introduced” Idaho Press. Jan. 24, 2025 ⤶ ⤶ ⤶
- ”Idaho HB58” BillTrack50. Introduced Jan. 24, 2025 ⤶ ⤶
- ”Idaho HB138” BillTrack50. Crossed over Feb. 19, 2025 ⤶ ⤶ ⤶
- ”October 2024 Medicaid & CHIP Enrollment Data Highlights” , Medicaid.gov, Accessed Jan. 30, 2025 ⤶ ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, Medicaid.gov, Accessed February 2025 ⤶
- “Medicaid Enrollment and Unwinding Tracker”, KFF.org, Accessed Jan. 30, 2025 ⤶ ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed Jan. 30. 2025 ⤶ ⤶

