
Medicaid eligibility and enrollment in Maryland
Maryland automatically enrolled 27,000 people in QHPs after they lost Medicaid during “unwinding” and didn’t pick their own new plan.

Who is eligible for Medicaid in Maryland?
Maryland’s Medicaid program, which is also called Medical Assistance, has higher income limits than many other states when it comes to Medicaid eligibility for children and people who are pregnant. Individuals with family income up to the following levels are eligible for Medicaid (note that these limits include the build-in 5% income disregard that’s used for MAGI-based Medicaid eligibility):
- 322% of the federal poverty level (FPL) for children ages 0-18
- 264% of FPL for someone who is pregnant (coverage continues for 12 months after the baby is born)
- 138% of FPL for parents and other adults
- Aged, blind, and disabled (ABD) individuals may also qualify for Medicaid; see the income and asset guidelines in the FAQs of the Maryland Department of Health and Mental Hygiene website.
- Maryland helps pay for long-term care for qualifying individuals; see the eligibility criteria and application information.
For ease of reference, the Maryland Health Connection website shows the monthly income limits in terms of dollar amounts rather than percentage of FPL.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Maryland
Apply online. Apply in person at a local health department or social services office. Call 1-800-456-8900 and have an application mailed to you. For help applying, call 1-855-642-8572 (1-855-642-8573 for individuals who have hearing difficulty).
Eligibility: Children ages 0-18 with household income up to 317% of FPL. Pregnant women with household income up to 250% of FPL. Adults with household income up to 138% of FPL. Aged, blind, and disabled (ABD) individuals: see income and asset guidelines. See the eligibility criteria for long-term care.



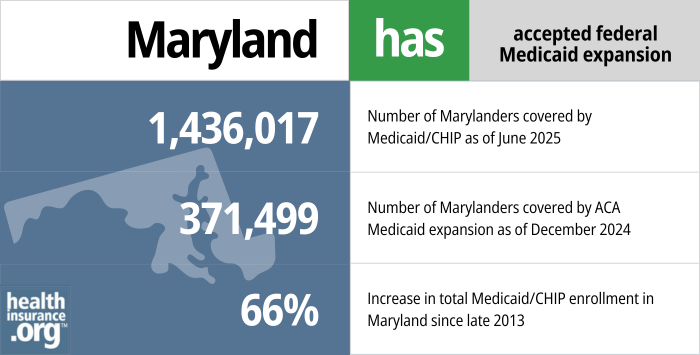
Did Maryland expand Medicaid under the ACA?
Yes, Maryland expanded Medicaid under the ACA. The state’s Medicaid expansion was authorized in May 2013 for a Jan. 1, 2014, start date. Medicaid expansion, which makes Medicaid available to low-income adults under age 65, is one of the Affordable Care Act’s main tenets to reduce the nation’s uninsured rate.
- 1,436,017 – Number of Marylanders covered by Medicaid/CHIP as of June 20251
- 371,499 – Number of Marylanders covered by ACA Medicaid expansion as of June 20242
- 66% – Increase in total Medicaid/CHIP enrollment in Maryland since late 20133
Explore our other comprehensive guides to coverage in Maryland

The ACA Marketplace allows individuals and families to shop for and enroll in ACA-compliant health insurance plans. Subsidies may be available based on household income to help lower costs.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Maryland.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Maryland as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Maine Medicaid eligibility and enrollment
How do I enroll in Medicaid in Maryland?
In general, you can enroll for Maryland Medicaid online or in person. See below for specifics, which vary for different eligible groups.
- If you are under 65 and don’t have Medicare, apply online at www.MarylandHealthConnection.gov.
- Seniors and people who have Medicare can apply for Medicaid using this website.
- Get an application or apply in person at a local health department or social services office. Call 1-800-456-8900 and have an application mailed to you.
- For help applying, call 1-855-642-8572 (1-855-642-8573 for individuals who have hearing difficulty)
- People who are pregnant are encouraged to apply at a local health department. Call 1-800-456-8900 for information
How does Medicaid provide assistance to Medicare beneficiaries in Maryland?
Many people with Medicare receive help through Medicaid with Medicare premium costs, prescription drug expenses, and expenses that Medicare doesn’t cover — such as long-term care.
Our guide to financial resources for Medicare enrollees in Maryland provides an overview of those programs, including Medicare Savings Programs, nursing home benefits, and income guidelines for assistance.
How did Maryland handle Medicaid renewals after the pandemic?
From March 2020 through March 2023, states were prohibited from disenrolling people from Medicaid, even if they no longer met the eligibility requirements. That rule ended March 31, 2023, and states began disenrolling people from Medicaid after the three-year pause.
Maryland began sending out Medicaid renewal packets in April 2023, and the first round of disenrollments came at the end of May. The state wrapped up the “unwinding” process in April 2024, and was among the states where the smallest percentage of people lost Medicaid during the unwinding process.4 After Maryland’s unwinding process was complete, Medicaid enrollment was still higher than it had been pre-pandemic, by more than 262,000 people.4
Net enrollment in Maryland Medicaid only declined by 6.4% during the unwinding period, versus a national average of 13.9%.5 And of the people whose Medicaid coverage was renewed in Maryland, 74% were renewed automatically (ex parte), without the enrollee needing to provide any additional information to the state.6
People who were no longer eligible for Medicaid could transition to a plan offered by an employer if one was available to them. But Maryland Health Connection (the state-run exchange/Marketplace) automatically enrolled people into private qualified health plans if they were no longer eligible for Medicaid and didn’t pick their own replacement plan. The person had the option of accepting that plan, picking a different plan, or canceling the plan if they had coverage elsewhere.
By April 2024, CMS reported that 48,976 Maryland residents had transitioned from Medicaid to a Marketplace plan during the unwinding period, including more than 27,000 who were automatically enrolled in a Marketplace plan.7
Does Maryland Medicaid provide dental benefits for adults?
Yes, as of 2023, Maryland Medicaid includes adult dental benefits. Prior to 2023, since the early 1990s, Maryland had not provided coverage for adult dental care through its Medicaid program (most states provide at least limited or emergency dental coverage for adults enrolled in Medicaid; Maryland was one of just three states that provided no coverage at all). But legislation (HB6 and SB150) was enacted in 2022 to add an adult dental benefit to the state’s Medicaid program as of 2023.
Children with Medicaid already had coverage for dental care in Maryland, as is the case nationwide. And Maryland did implement a program in 2019 to provide dental benefits to Maryland residents age 21-64 who were dually enrolled in Medicaid and Medicare (ie, they are disabled and have low incomes and low assets). But the state estimated that fewer than 39,000 people would be eligible for benefits under that program. Under HB6/SB150, a far larger population of low-income residents gained access to dental care starting in 2023.
Maryland Medicaid history and details
Maryland Medicaid enrollment and managed care
Medicaid enrollment in Maryland has grown significantly over the last several years. From late 2013 to early 2024, total enrollment in Maryland’s Medicaid/CHIP grew by 88%.8
Total Medicaid enrollment in Maryland stood at almost 1.7 million people in mid-2024, after the state had rechecked all enrollees’ eligibility post-pandemic.4
Maryland has used Medicaid-managed care since 1991. As of 2022, Medicaid Managed Care Organizations (MCOs) covered about 90% of Maryland’s Medicaid population, while the other 10% were covered under the Medicaid Fee for Service program (the Medicaid FFS program includes elderly enrollees who are also eligible for Medicare, and those who are in long-term care facilities).
There are currently nine health insurance carriers that participate in Maryland’s Medicaid Managed Care program:
- Aetna Better Health
- CareFirst BlueCross Blue Shield Community Health Plan
- Jai Medical Systems
- Kaiser Permanente
- Maryland Physicians Care
- MedStar Family Choice
- Priority Partners
- UnitedHealthcare
- Wellpoint Maryland (formerly Amerigroup Community Care)
Maryland’s leadership and Medicaid expansion
Republican Larry Hogan took over as Maryland’s governor in January 2015, replacing Democrat Martin O’Malley. O’Malley faced a term limit and was not running for re-election; Lt. Gov. Anthony Brown vied with Hogan.
While Hogan frequently criticized O’Malley and Brown over Maryland’s state-run health insurance exchange, Medicaid expansion was not a campaign issue. In fact, Hogan acknowledged that significant changes to Medicaid were unlikely given Democrats’ dominance in the Maryland General Assembly.
Maryland gathered much information about the potential impacts of the ACA’s Medicaid expansion before proceeding with implementation, and the findings were summarized in a Health Affairs blog by an official with the Maryland Department of Health and Mental Hygiene. Maryland estimated that 190,000 Marylanders would gain Medicaid coverage through the expansion by 2020 and took note of a New England Journal of Medicine research showing a 6.1% reduction in mortality for low-income adults covered by expanded Medicaid. Maryland also learned that Medicaid expansion would have a significant positive effect on the state economy, including an estimated $25 billion in federal Medicaid funding and 27,000 new jobs by 2020.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.

Looking for more information about other options in your state?
Need help navigating health insurance options in Maryland?
Explore more resources for options in MD including ACA coverage, short-term health insurance, dental and Medicare.
Speak to a sales agent at a licensed insurance agency.
Footnotes
- “June 2025 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed October 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed October 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed October 2025 ⤶
- ”Maryland Department of Health recognized as a top state as it completes yearlong Medicaid redeterminations process” Maryland Department of Health. July 11, 2024 ⤶ ⤶ ⤶
- ”Medicaid Enrollment and Unwinding Tracker” KFF. Aug. 23, 2024. ⤶
- ”Medicaid Enrollment and Unwinding Tracker” KFF. Aug. 23, 2024. ⤶
- ”State-based Marketplace (SBM) Medicaid Unwinding Report” Centers for Medicare & Medicaid Services. Data through April 2024; Accessed Aug. 27, 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed Aug. 27, 2024 ⤶

