Medicaid eligibility and enrollment in Nebraska

Medicaid expansion took effect in October 2020; Nebraska abandoned its plan to have a work requirement for enhanced Medicaid benefits

Who is eligible for Medicaid in Nebraska?
Nebraska Medicaid (Heritage Health for most enrollees) coverage is available for the following populations:
- Adults under age 65 with income up to 138% of the poverty level, due to Medicaid expansion that took effect in Nebraska in 2020 (note that the eligibility requirements are more stringent for people who are 65 or older, or also enrolled in Medicare prior to age 65).
- Pregnant women with household income up to 199% of poverty.
- Children with household income up to 218% of poverty
Apply for Medicaid in Nebraska
You can enroll online at HealthCare.gov or use the call center at 1-800-318-2596. You can also enroll online at ACCESSNebraska, or print a paper application from their website.
Eligibility: Parents with dependent children are eligible with household income up to 57% of poverty. Pregnant women with income up to 194% of poverty, and children with income up to 213% of poverty.



Enrollment in expanded Medicaid took effect in 2020
Medicaid expansion – dubbed the Heritage Health Adult Program – took effect in Nebraska as of October 2020 (enrollment began on August 1, 2020), under the terms of the ballot initiative that was approved by the state’s voters in the 2018 election (details below).
Under the newly expanded eligibility rules, adults with income up to 138% of the poverty level are eligible for Medicaid in Nebraska. The state expected roughly 90,000 people to become newly eligible for Medicaid coverage in Nebraska under the expanded eligibility guidelines. By late 2022, enrollment in Nebraska’s expanded Medicaid had grown to 75,000 people.
Learn how states that expanded Medicaid might reduce spending on Medicaid.
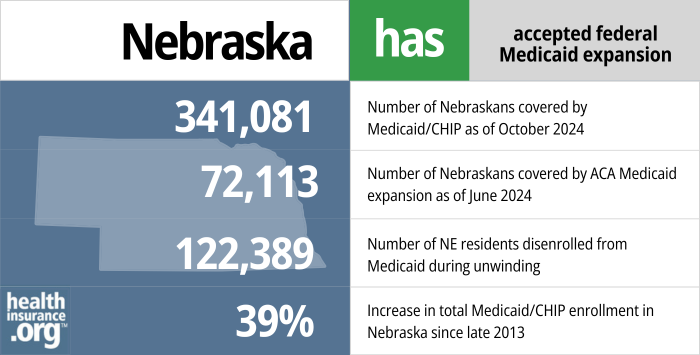
- 341,081– Number of Nebraskans covered by Medicaid/CHIP as of October 20241
- 72,113– Number of Nebraskans covered by ACA Medicaid expansion as of June 20242
- 122,389 – Number of NE residents disenrolled from Medicaid during unwinding3
- 39% – Increase in total Medicaid/CHIP enrollment in Nebraska since late 20134
Explore our other comprehensive guides to coverage in Nebraska

We’ve created this guide to help you understand the Nebraska health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Nebraska.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Nebraska as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

Frequently asked questions about Nebraska Medicaid
How do I enroll in Nebraska Medicaid?
You can submit an application for Medicaid at any time during the year. Applications can be made online or by phone.
If you are under 65 and don’t have Medicare:
- You can begin the process online at HealthCare.gov or by phone via the HealthCare.gov call center at 800-318-2596. If it looks like you’re eligible for Medicaid, HealthCare.gov will send your information to Nebraska Medicaid and they will contact you to complete the enrollment.
- You can also enroll online at ACCESSNebraska at any time.
- The Do I Qualify screening tool at ACCESSNebraska can help you determine which public programs you’re eligible for: You may be able to enroll in other benefits beyond Medicaid.
If you’re 65 or older or have Medicare:
-
- You can apply online using this website.
- You can apply by calling (855) 632-7633.
- You can apply by visiting a local Public Assistance office.
How does Medicaid provide financial assistance to Medicare beneficiaries in Nebraska?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Nebraska includes overviews of these programs, including Medicaid long-term care benefits, Extra Help, and eligibility guidelines for assistance.
How is Nebraska handling Medicaid renewals after the pandemic?
Medicaid disenrollments were paused nationwide for three years during the pandemic, but resumed in the spring/summer of 2023. Under federal rules, all Medicaid enrollees’ eligibility must be redetermined at some point in a year-long “unwinding” period that began in the spring of 2023.
By September 2023, nearly 47,000 people had been disenrolled from Nebraska Medicaid, while coverage had been renewed for nearly 109,000 enrollees who were determined to still be eligible for Medicaid. The Nebraska Department of Health and Human Services had expected that between 10% and 20% of the state’s Medicaid enrollees would no longer be eligible for coverage once the pandemic-era continuous coverage requirement ended.
Nebraska Medicaid enrollees should ensure that their contact information is up to date so that they’ll receive renewal communications from the state. This will continue to be the case even after the “unwinding” period ends; eligibility redeterminations will continue to be conducted on a monthly basis in the future, just as they were pre-pandemic.
Enrollees can log into their ACCESSNebraska account to do this, or call Nebraska Medicaid at (855) 632-7633. The state is attempting to reach people by multiple methods, including phone calls as well as mail. But coverage will be discontinued if the state is unable to redetermine a person’s eligibility, which could result in a gap in access to medical services. So it’s important to keep contact information updated and also respond quickly to any request for information from the Nebraska Medicaid program.
Many people who are disenrolled from Medicaid will be eligible to enroll in an employer’s plan, and some will be eligible for Medicare. But for people who need to obtain their own replacement coverage (ie, they aren’t eligible for Medicare or an employer’s plan), HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through July 31, 2024, for anyone who loses Medicaid at any time during that window.
Legislation impacting Nebraska Medicaid
Medicaid expansion: Voters said yes in 2018, but implementation was delayed until late 2020
After lawmakers in Nebraska rejected Medicaid expansion for six years, proponents of Medicaid expansion took the issue to the state’s voters in the 2018 election.
Nebraska State Senator Adam Morfeld (D-Lincoln) introduced Legislative Resolution 281CA during the 2018 session, calling for a constitutional amendment to be on the ballot, declaring health care a right and expanding Medicaid in Nebraska. But that measure did not advance in the Health and Human Services Committee.
Instead, supporters began working on a ballot initiative that would propose a Medicaid expansion law, instead of a constitutional amendment (in Nebraska, 7% of voters must sign a petition to get a proposed law on the ballot, as opposed to 10% for a constitutional amendment). Medicaid expansion proponents began collecting signatures in March 2018, and successfully gathered enough signatures; the Nebraska Secretary of State confirmed in late August that Medicaid expansion would be on the ballot in Nebraska in November 2018. A judge rejected efforts by Nebraska GOP Senators who tried to block the ballot initiative based on “procedural, statutory and constitutional flaws.”
Nebraska Initiative 427 passed with 53% of the vote. It required the state to expand Medicaid as called for in the ACA (ie, to people earning up to 138% of the poverty level). According to the terms of the initiative, the state had to submit an expansion plan to the federal government by April 1, 2019.
On April 1, the Nebraska Department of Health and Human Services announced the details of their Medicaid expansion proposal, and also submitted their state plan amendments to the federal government. The state has also maintained a web page with a variety of information about the Medicaid expansion process. But then-Governor Pete Ricketts had long opposed Medicaid expansion, and while his administration did implement the voter-approved Medicaid expansion, they did so on a very delayed timeline—a fact that Ricketts made clear soon after the ballot initiative passed. (For perspective, voters in Utah and Idaho approved Medicaid expansion at the same time, and expanded coverage in those states took effect in January 2020.)
The Ricketts administration also initially rolled out a two-tiered system, with enhanced benefits (dental, vision, and over-the-counter medication coverage) available for enrollees who participate in care management and, starting in the second year of the program, fulfill a community engagement/work requirement that was approved by the Trump administration in October 2020 (this is described in more detail below). But that program was terminated by the state in 2021, after the Biden administration made it clear that work requirements would not be allowed. So as of October 2021, all Medicaid expansion enrollees in Nebraska have the enhanced benefits package.
Nebraska initially had two tiers of Medicaid expansion coverage, but the state terminated that approach in 2021 and all enrollees now receive the enhanced benefits
Although lawmakers in Utah and Idaho passed legislation in 2019 to adjust the terms of the Medicaid expansion ballot initiatives that voters had passed in those states, Nebraska lawmakers did not (and they did include funding for the state’s share of the cost of the first nine months of Medicaid expansion in the budget that was signed by Ricketts in May 2019).
Instead, the Nebraska-specific modifications to Medicaid expansion — which are no longer in effect — came from former Governor Ricketts’ administration. While the modifications were not as draconian as those implemented in some other states, Nebraska was still deviating from the version of Medicaid expansion called for in the ACA and approved by the state’s voters, and was adding administrative cost and complexity.
To expand Medicaid, Nebraska added the Heritage Health Adult Program to its existing Heritage Health Program. An 1115 waiver proposal for the final version of the state’s Heritage Health plan was submitted to CMS in December 2019 for federal review. It was approved by CMS in October 2020, a few weeks after Medicaid expansion took effect in the state. Nebraska posted a series of FAQs about the newly approved waiver, which took effect in April 2021 (the work requirement was slated to take effect in April 2022, but the waiver program was terminated prior to that, so the work requirement never took effect).
Under the state’s approved waiver, the Heritage Health Adult Program would have a basic level of coverage, modeled after the Blue Cross Blue Shield Pride plan, which is one of the largest small-group plans in Nebraska. All residents who are eligible for expanded Medicaid would qualify for at least the Basic Coverage.
Enrollees would be able to qualify for Prime Coverage (including coverage for dental, vision, and over-the-counter medications) starting in the spring of 2021 if they meet additional requirements: To receive Prime Coverage in the first year, enrollees had to participate in care and case management, select a primary care provider, and have an annual checkup. Starting in year two (ie, April 2022 and beyond), keeping Prime Coverage would have required enrollees to fulfill an 80-hour-per-month work requirement (eg. working, going to school, volunteering for a public charity, serving as a caregiver for a relative).
In order to retain eligibility for Prime Coverage, members would also have been required to promptly notify the state Medicaid department of any pertinent changes in circumstances, and would have had to avoid missing medical appointments without notifying the doctor’s office. Members who miss three or more medical appointments without notifying the doctor’s office would have been locked out of Prime Coverage for the remainder of their current six-month coverage period and for the next two coverage periods.
According to the state’s proposal, Nebraska officials expected nearly a third of the newly eligible population to qualify for only the Basic benefits.
Not surprisingly, the different levels of coverage (ie, traditional Medicaid for pregnant, disabled, and elderly adults, Basic Coverage for some adults, and Prime Coverage for other adults) were expected to significantly increase administrative costs for Nebraska’s Medicaid program.
Nebraska’s waiver proposal also sought federal permission to eliminate retroactive eligibility for most Heritage Health Adult Program enrollees, and instead grant coverage no earlier than the first of the month the application is submitted. But CMS did not approve this part of the proposal, which would have cost hospitals a significant amount of money.
Ultimately, the Biden administration took a different approach to Medicaid work requirements, and began notifying states in early 2021 that work requirements were essentially incompatible with the overall Medicaid mission. By late 2021, the Biden administration had withdrawn approval for Medicaid work requirements in all states where the prior administration had approved them. Due to the changing federal regulations, Nebraska requested that the Heritage Health Adult waiver demonstration be terminated in mid-2021. And as of October 2021, all Medicaid expansion enrollees in Nebraska began receiving Prime Coverage, with no strings attached.
Pre-2018 efforts to expand Medicaid via legislation were unsuccessful
In 2013, LB577, which would have created a modified Medicaid expansion program, was rejected by the legislature in Nebraska. A year later, the Wellness in Nebraska Act (LB887) was introduced in January 2014 by Senator Kathy Campbell, but it didn’t pass during the 2014 legislative session, and was indefinitely postponed in April 2014.
The Wellness in Nebraska Act would have expanded traditional Medicaid to people with incomes up to the poverty level (those who are currently in the coverage gap), and would have relied on federal Medicaid funding to purchase private coverage for people with incomes between 100% and 138% of poverty. Several states are using waivers to implement unique approaches to Medicaid expansion, and New Hampshire and Arkansas both use waivers purchasing private coverage for at least some Medicaid enrollees.
In 2015, lawmakers introduced Legislative Bill 472 to expand Medicaid, but it did not pass out of committee. Also in 2015, two professors from the University of Nebraska-Kearney published the results of a study that found that expanding Medicaid would result in significant financial benefits for the state. After exhaustive study, the researchers concluded that expansion of Medicaid “passes a rigorous cost/benefit analysis.”
In January 2016, Nebraska State Senator John McCollister (R, Omaha), introduced Legislative Bill 1032 in an effort to expand Medicaid in Nebraska. McCollister had been leading the push for Medicaid expansion in the state for almost a year at that point, but his legislation failed to advance out of committee.
LB1032 would have been a privatized approach to Medicaid expansion, similar to the system Arkansas implemented in 2014, and New Hampshire implemented in 2016 (New Hampshire has abandoned the private approach, however, and switched to Medicaid managed care). LB1032 also included optional education and job skills training for Medicaid enrollees, in an effort to help them transition to higher-paying jobs and away from public assistance programs like Medicaid.
In early discussions, then-Governor Ricketts reiterated his opposition to Medicaid expansion, including the privatized version proposed in LB1032. Conservative lawmakers were opposed to LB1032 as well, ultimately dooming it. The 2016 legislative session ended in Nebraska with no progress towards Medicaid expansion or closing the state’s coverage gap.
And in 2017, just before the start of the Trump Administration, Sen. Morfeld introduced LB441, which called, yet again, for Medicaid expansion in Nebraska. But a legislative committee decided to take no action on the bill in the spring of 2017, as the state waited to see what would happen in terms of health care reform at the federal level (at that point, ACA repeal bills were still very much under consideration in Congress, although they all ultimately failed later in 2017).
Nebraska Medicaid enrollment numbers
From the fall of 2013 through July 2016, total net enrollment in Nebraska’s Medicaid program actually declined by 9,764 people, which amounted to a decrease of 4%. By early 2020, however, enrollment was back to nearly where it had been in 2013, with only 188 fewer enrollees. And by June 2023, enrollment was 62% higher than it had been in 2013, due in large part to Medicaid expansion and the continuous coverage rules that were in place during the COVID pandemic. Enrollment had started to decline again by that point however, due to the end of the continuous coverage rule. By September 2023, about 47,000 people had been disenrolled from Nebraska Medicaid, and total enrollment in the program stood at 365,299.
Coordinated system has three managed care organizations
As of 2013, nearly 76% of Nebraska’s Medicaid enrollees were in managed care programs run by Aetna, AmeriHealth, and UnitedHealthcare. The state overhauled its Medicaid managed care system in 2016, and managed care contract bids were submitted by six carriers in early January.
The overhauled program is called Heritage Health, and it combines coverage (for Medicaid and CHIP) of physical health, behavioral health, and pharmacy care into one coordinated system. The new system took effect January 1, 2017. Three carriers were awarded contracts to serve as managed care plans under Heritage Health:
- Nebraska Total Care (Centene)
- UnitedHealthcare Community Plan
- Healthy Blue (previously Wellcare of Nebraska)
Nebraska Medicaid history
Nebraska implemented Medicaid in July 1966, just a few months after the first wave of states did so in January of that year.
The federal match rate for Medicaid (the portion that the federal government pays, in addition to what the state pays) is tied to the per capita income in the state, and rising incomes in Nebraska mean that the federal match rate for Medicaid costs decreased from 53.27% to 51.16% in 2016.
This was the lowest federal match rate in the history of Nebraska’s Medicaid program, and the impending decrease led the Nebraska Department of Health and Human Services to request $76 million from the legislature in October 2014, to cover the anticipated budget shortfall over the upcoming two fiscal years.
By fiscal year 2018, Nebraska’s federal match rate had increased slightly, to 52.55%.
To address the COVID-19 pandemic, the Families First Coronavirus Response Act gave states an additional 6.2% in federal matching funds for Medicaid. This is being phased out throughout 2023, however, and there will no longer be a pandemic-related Medicaid funding bump as of 2024.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- “October 2024 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed January 2025 ⤶
- “Medicaid Enrollment – New Adult Group”, Medicaid.gov, Accessed February 2025 ⤶
- ”Medicaid Enrollment and Unwinding Tracker“, KFF.org, January 2025 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2025 ⤶

